INTRODUCTION
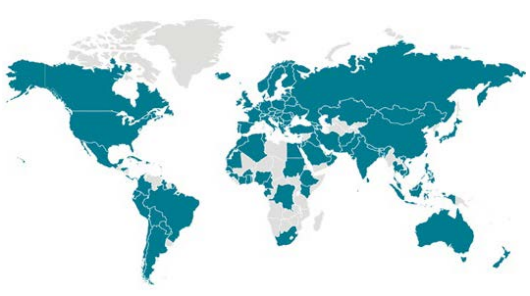
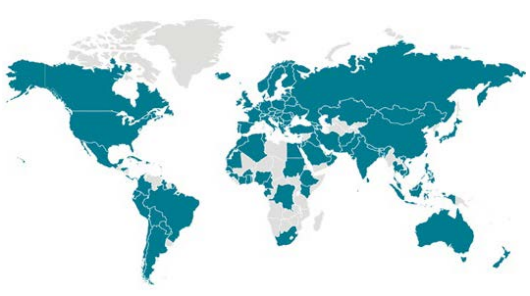
In this special editorial we discuss the ways in which global public health professionals can support other public health, medical, laboratory, health education, and emergency management professionals responding to the coronavirus disease-2019 (COVID-19) pandemic. The World Health Organization (WHO) assigned a Global WHO Risk Assessment Level of “Very High” to the treatment of COVID-19.1 Globally, the responses of governments to COVID-19 have been containment and mitigation where the disease is present. On March 2nd, 2020, there were 88,948 confirmed cases. The number of cases has only increased since that time, and on March 11th, 2020, WHO declared COVID-19 as pandemic.2 As of March 26th, 2020,3 WHO has reported the following (see Table 1):
| Table 1. Situation in Numbers as of March 26, 2020 |
|
Total (new) cases in last 24-hours
|
| Globally |
462,684 confirmed (49,219); 20,834 deaths (2,401) |
| Western Pacific Region |
99,058 confirmed (1,292); 3,540 deaths (22) |
| European Region |
250,287 confirmed (29,771); 13,950 deaths (1,964) |
| South-East Asia Region |
2,536 confirmed (192); 79 deaths (7) |
| Eastern Mediterranean Region |
32,442 confirmed (2,811); 2,162 deaths (154) |
| Region of the Americas |
75,712 confirmed (14,878); 1,065 deaths (252) |
| African Region |
1,937 confirmed (275); 31 deaths (2) |
| These data illustrate the global nature of the pandemic. |
BACKGROUND
The definition of the disease follows: COVID-19 is the infectious disease caused by a recently discovered coronavirus. This new virus and disease were unfamiliar before the outbreak began in Wuhan, China, in December 2019.4 COVID-19 is a new strain of coronaviruses not previously identified in humans (note: coronaviruses are zoonotic -transmitted between animals and people). COVID-19 is a highly infectious respiratory disease caused by the SARS-COV-2 virus, and is currently associated with high rates of morbidity and mortality in all the regions of the WHO.5 The situation of COVID-19 is an example of how a public health problem in one country affects many others outside the borders of the initial country.6
COVID-19 is one of seven viruses in the family of human coronaviruses.7 The common cold is linked to four types of coronaviruses (229E, NL63, OC43, AND KHU1). Other severe types of this family of viruses includes severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). The current, COVID-19 strain had never been seen in the human population prior to late-December 2019; COVID-19 is considered a novel coronavirus.
The most common symptoms of COVID-19 include fever, tiredness, and dry cough; additional symptoms are aches and pains, nasal congestion, runny nose, sore throat or diarrhea.4 The WHO has reported that older people and those with underlying medical problems (e.g., high blood pressure or diabetes) have been more likely to develop serious illness.
Even if not directly involved in COVID-19 public health activities, the role of global public health professionals could include keeping up-to-date with current facts that can be useful to community leaders in support of national, public health activities designed to control and mitigate the disease.
Public Health Action: Supporting Our Peers and Communities
There is no vaccine for COVID-19. Therefore, as global public health professionals, it is important for us to recall the basic public health prevention strategies that are available for all types of human coronaviruses to prevent respiratory illnesses. It is equally important for us to share this knowledge with others. Please see the following list of prevention strategies which we can share with communities where we live7:
- Wash your hands often with soap and water for at least 20 seconds, and help young children do the same. If soap and water are not available, use an alcohol-based hand sanitizer. Wash your hands especially after coughing and sneezing, before and after caring for an ill person, and before preparing foods and before eating.
- Cover your nose and mouth with a tissue when you cough or sneeze and then throw the tissue in the trash.
- Avoid touching your eyes, nose, or mouth with unwashed hands.
- Avoid close contact (such as kissing, sharing cups, or sharing eating utensils) with people who are sick.
- Clean and disinfect frequently touched surfaces and objects, such as toys and doorknobs, especially if someone is sick.
- Stay home when you are sick, except when you need to get medical care.
- Wash hands after animal contact and after visiting farms, markets, barns, petting zoos, and agricultural fairs.
- Avoid contact with animals who are sick.
Given the current, Global WHO Risk Assessment Level for COVID-19, global public health professionals can help our local communities with specific actions. First, we can keep “up-to-date” with the current facts of COVID-19 from Official Government sources in the countries where we live and from reference institutions and organizations. Second, we can share prevention strategies, like those above, with family, friends, and co-workers in an understandable and calm manner. Third, we can help local decision-makers (e.g., school leaders, businesses, community leaders) think about public health data and information pertaining to the COVID-19 experience in a specific location and reasonable ways to keep people healthy while continuing operations in support national government and subnational government efforts to confront the spread of COVID-19. Fourth, we can arrange health science gatherings (when safe) for all professionals where we can strategize on efforts to address the COVID-19 pandemic and its aftermath. Finally, we can be a calm and credible voice in our communities to help leaders strategize how best to protect the population from COVID-19 while continuing the operations of the community (Boxes 1 and 2).
| Box 2.
Preparing for a Pandemic: What Individuals Should Do
Before a Pandemic:
• Store a two three-week supply of water and food.
• Periodically check your regular prescription drugs to ensure a continuous supply in your home.
• Have any nonprescription drugs and other health supplies on hand, including pain relievers, stomach remedies, cough and cold medicines, fluids with electrolytes, and vitamins.
• Get copies and maintain electronic versions of health records from doctors, hospitals, pharmacies and other sources and store them, for personal reference. Get help accessing electronic health records.
• Talk with family members and loved ones about how they would be cared for if they got sick, or what will be needed to care for them in your home.
During a Pandemic
Limit the Spread of Germs and Prevent Infection
• Avoid close contact with people who are sick.
• When you are sick, keep your distance from others to protect them from getting sick too.
• Cover your mouth and nose with a tissue when coughing or sneezing. It may prevent those around you from getting sick.
• Washing your hands often will help protect you from germs.
• Avoid touching your eyes, nose or mouth.
• Practice other good health habits. Get plenty of sleep, be physically active, manage your stress, drink plenty of fluids, and eat nutritious food.
• Clean & disinfect frequently touched surfaces daily. This includes tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, nozzles, and sinks.
From: Ready. Gov (Web site: https://www.ready.gov/pandemic. Accessed: March 11, 2020) |
CONCLUSION
Our “front-line” peers combating the spread of COVID-19 have “their hands full”, and we are grateful for their service to our society. Those of us not directly involved in “front-line” efforts can still help by supporting our peers. We can share up-to-date COVID-19 facts and information with community leaders and businesses. We can be a calm and credible voice in our communities to help leaders strategize how best to protect the population from COVID-19 while continuing the operations of the community. And we can show the members of our communities what to do during the COVID-19 pandemic by our personal example.
We attest: The COVID-19 pandemic is a major concern for the readership of this journal. All of us are concerned with the containment, mitigation, and prevention of COVID-19 in our communities. We encourage global public health professionals, where possible and safe, to help and collaborate with official, organized actions in local communities to contain the spread of COVID-19.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.