INTRODUCTION
The clinical features of the Prader–Willi Syndrome (PWS) are complex, variable and characterized by severe neonatal hypotonia, feeding problems, childhood-onset hyperphagia, obesity, short stature, cranio facial disharmony, hypogonadism, learning and behavioral difficulties (because of hypothalamus dysfunction). Clinical features may alter with age. Scoliosis, hypopigmentation of skin and hair, juvenile diabetes, narrow forehead, sleep apnoea (because of obesity), delayed healing, small hands and feet and self inflicted injuries are some of the other characteristic features of this syndrome.1,2
The worldwide incidence is between 1:15000 and 1:50000. It usually affects both males and females equally with a large preponderance for boys. Oro-facial manifestations reported in PWS include almond-shaped eyes with up-slanting palpebral fissures and a triangular mouth.3 Intraoral findings include the presence of hypoplastic enamel, rampant caries, low basal salivary secretion, delayed tooth eruption and excessive tooth wear.4-8
CASE REPORT
A 6-year-old boy reported to the Department of Paedodontics and Preventive Dentistry, Sudha Rustagi College of Dental Sciences, Faridabad, with the chief complaint of multiple decayed teeth since 2-3 years with no associated pain or swelling. The case was referred to us by the Fortis Hospital, Faridabad.
Natal history stated that the child was delivered by Caesarean section with the cord twisted around his neck and aspirated meconium. The patient did not cry at the time of birth and was kept in an incubator for a week. Prenatal history was not significant.
He had pneumonia and respiratory distress at 7 months of age and hospitalized for the same. Milestones were delayed. There were history of seizures since the age of 3 years and the patient was under medications for the same. Speech impairment and intellectual disability were also seen. He had been diagnosed with right undescended testes for which he was surgically operated in July 2011 and March 2012 but the surgery was unsuccessful.
Family history: The boy was the youngest of three siblings with 2 elder sisters who were normal and no history of any disorder running in family.
Personal history: The child was very particular about personal hygiene and was having a routine of brushing once daily in the morning using toothbrush and toothpaste.
CLINICAL MANIFESTATIONS
On clinical examination, the child was short statured and obese (Figure 1). His height was 105 cms (whereas another child of same age is 119 cms) with a BMI (Body Mass Index) (weight [kg]/height [m2]) of 24.1.

Figure 1: Short statured obese child.
The boy had up-slanting palpebral fissures, almond shaped eyes, hypertelorism and mild strabismus. Line joining lateral canthus and superior point of pinna on left side was lower (Figure 2).
Figure 2: Upslanting palpebral fissures, almond shaped eyes, hypertelorism and mild strabismus.
Thin upper lip and down turned corners of the mouth gave a ‘fish mouth appearance’ (Figure 3). His hands and feet were small (Figure 4) and self inflicted injuries were present on hands (Figure 5).

Figure 3: Fish mouth appearance.

Figure 4: Small hands and feet.

Figure 5: Self inflicted injury.
INTRAORAL FINDINGS
- Early mixed dentition stage.
- Dental caries were present in teeth 53, 63, 64, 65, 73, 75, 83 and 85.
- Root stumps were present with respect to 51, 52, 54, 61, 62, 72, 74, 82 and 84.
- Anterior cross bite between 11 and 41.
- No abnormality detected in frenal attachments, tongue, buccal mucosa, palate, floor of the mouth.
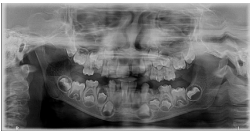
- Panoramic radiograph showed presence of all permanent teeth (Figures 6-9).

Figure 6: Intraoral photograph showing carious teeth and root stumps.

Figure 7: Intraoral photograph showing anterior crossbite.

Figure 8: Intraoral photograph showing gingival hypertrophy.
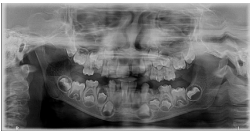
Figure 9: Panoramic radiograph showing all permanent teeth.
MAJOR DIAGNOSTIC CRITERIA
In spite of history of rapid weight gain at the age of 3 ½ years, the child was cheerful and good natured but exhibited behavioral problems such as, short attention span, temper tantrums, obsessive compulsive disorder and stubbornness. Rage-type response of behavior was noticed during extraction of teeth, hyperphagia, narrow bifrontal diameter, almond-shaped eyes, down turned corners of the mouth, hypogonadism and thick viscous saliva. Delayed healing of wounds was reported after extraction of teeth.
CONFIRMATORY DIAGNOSIS
This syndrome has similarity to various conditions like Down`s syndrome, Growth hormone deficiency, Obsessive compulsive disorder and Obstructive sleep apnea syndrome. Multiple consultations from doctors were taken and genomic imprinting suggested at the age of 3 years. Gene mapping was performed and the diagnosis was confirmed.
TREATMENT PLAN
- Restorations of carious teeth 53, 63, 65, 73, 75, 83 and 85.
- Extractions of root stumps 51, 52, 54, 61, 62, 72, 74, 82 and 84 followed by space maintainers.
- Pulpectomy 64.
- Anterior cross bite correction.
TREATMENT RENDERED
- Caries excavation done and GIC restorations.
- Pulpectomy.
- Extractions were performed.
- Patient is still under follow up.

Figure 10: Post treatment photograph of patient.
DISCUSSION
Management of PWS requires multidisciplinary care that includes combination of behavioural therapy, early diet managements, speech therapy, routine preventive health care with exercises and medications (such as growth hormone replacement therapy).1
Different case studies also manifested classical features of the syndrome by assessing various parameters.
Salako et al8 reviewed the oral findings of children with PWS and found that oral mucosa in such cases is prone to self inflicted injuries because of having the habit of picking at the skin and biting the oral mucosa.
Olczak-Kowalczyk et al6 assessed the presence of self inflicted injuries in such children either as picking of the skin or biting of the oral mucosa.
Saeves R et al3 evaluated the orofacial dysfunction (present in 87%), resulting in chewing difficulties, increased prevalence of oral habits and drooling of foamy and viscous saliva. Severe respiratory problems and snoring was frequent.
CONCLUSION
Early diagnosis and thorough orofacial examination of such cases is important to optimize treatment planning and management and to minimize the risk of progression of developing symptoms. Once the diagnosis of syndrome is confirmed, dental consultations should be started, in which education of the parents on the possible dental problems and instructions on how to prevent them should be given. Early introduction of good dietary and oral hygiene practices and use of fluoride supplements, when appropriate, would help prevent the deleterious dental consequences, as experienced here in this case report. Early interventions also include physical and occupational speech therapy. Therapeutic interventions to manage growth, regular exercises, dietary and behavioral concerns can enhance the child’s potential and can cause a significant impact on health.
ETHICAL APPROVAL
This case study protocol was approved by the Regional Medical Research Ethics Committee and also from the Ethical Committee of same institute where the case study was performed. Informed consent was obtained from parents of the child.
CONFLICTS OF INTEREST
None.