INTRODUCTION
Disasters involving chemical release are of concern in our modern industrialized world with highly urbanized cities because of the propensity of such incidents for causing injury and death in large numbers such as the Bhopal disaster1 in India in 1984. In our present times of prevailing low intensity conflicts and terrorism-linked events, there is an increasing necessity for medical preparedness in dealing with these situations. The Sarin Incident in Tokyo and Matsumoto,2,3,4 demonstrated the impact of mass casualty incidents from chemical terrorism using chemical warfare agents released by simple improvised chemical dispersion methods on an unsuspecting civilian population. Most patients from this incident presented promptly to the nearest emergency departments (ED) with no pre-hospital or hospital decontamination resulting in significant secondary contamination of emergency rescue and hospital personnel. Our local experience5,6,7 in chemical disasters demonstrated the impact on hospital personnel when over a third of healthcare providers on duty including all responding trauma team members developed secondary symptoms from managing tear gas contaminated casualties with no prior decontamination. Bearing this in mind, all public hospitals in Singapore were tasked by the health authorities to prepare for hazardous materials disasters and had to be equipped to deal with managing contaminated casualties and the decontamination of these victims to reduce toxic exposure to the victims and address the potential spread of contamination to limit damage from secondary exposure of healthcare providers and secondary contamination of healthcare facilities. Most healthcare systems depend on the fire services which predominantly uses the traditional ladder pipe system set up for decontamination of mass casualties.8 There have been innovative approaches to dealing with this situation including a recent study Imamedjian et al9 trialling the use of public buses and tents as holding areas and decontamination facility. The stark challenges of acute care hospitals in the United Kingdom10 to be prepared to perform mass decontamination are well-documented from lack of critical infrastructure, logistics, manpower and consistent regular training to maintain competency amongst healthcare providers. In the Singapore context, we have been using our tried and tested rapid deployment hospital decontamination station (HDS) located near to the ED for the last two decades. This article reviews the unique features of this entity.
Unique Features of the Hospital Decontamination Station (HDS)
Singapore General Hospital (SGH), was the first institution in Singapore to take on the challenge to innovate and build the HDS which set the precedent for all other local institutions. The Department of Emergency Medicine (DEM) celebrated its 70th anniversary in 2018. It is an opportune moment to acknowledge one of its pioneer achievement’s; the hospital decontamination station (HDS), an important innovative facility the first of its kind in Singapore. The HDS was built in the early part of this millennium and was intended as a medical countermeasure to the rising threat of chemical terrorism and industrial chemical accidents to decontaminate chemically contaminated casualties arriving at the hospital from the disaster scene at short notice. We describe the special considerations that went into constructing the HDS that makes it stand out as a significant countermeasure addressing the unique challenges of dealing with hazardous materials disasters with contaminated casualties by its timely deployment.
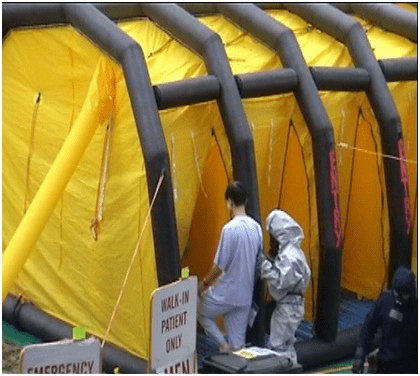
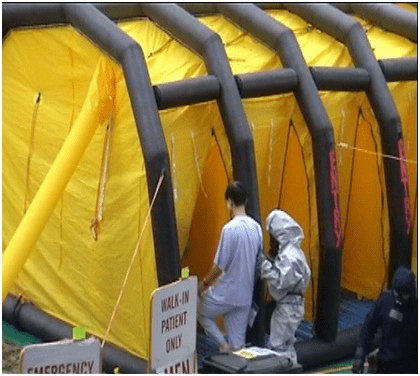
Lessons from the past, both local and overseas, have shown the rapid escalation of chemical disasters with mass casualties. The likelihood of setting up pre-hospital decontamination during disasters by rescue services in most modern-day built up cities which are gridlocked with traffic congestion and high population density is low. It is appreciated that prompt deployment of such decontamination facilities to deal with contaminated casualties who are likely to arrive in large numbers at short notice with no prior decontamination at scene is paramount to successful management of such scenarios. In this regard,the HDS (Figures 1A, 1B and 1C), a semi-automatic decontamination facility located in proximity just outside the entrance of the Emergency Department (ED) that could be operational within 5-minutes of activation by a single staff member is purpose fit. The alternative approach in the past using mobile commercial decontamination systems (Figure 2) took 45-minutes to deploy with specially trained manpower. The space constraints in storing these commercial decontamination sets, retrieving it when required for deployment and short shelf life are additional limitations.
Figure 1A. Ambulance Parking Bay Immediately Outside the Department of Emergency Medicine (DEM) Entrances

Figure 1B. Deployment of Hospital Decontamination Station (HDS) Shower Curtains

Figure 1C. Hospital Decontamination Station (HDS) in Full Deployment

Figure 2. Commercial Mobile Decontamination Shower for Ambulatory Casualties
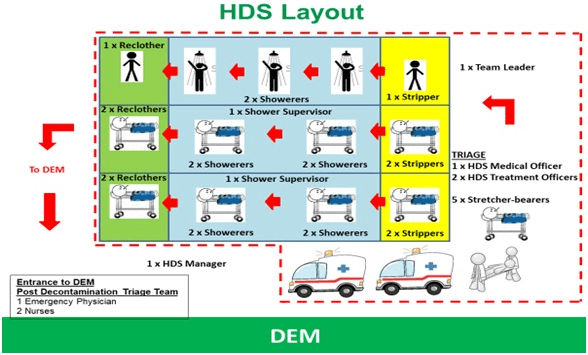
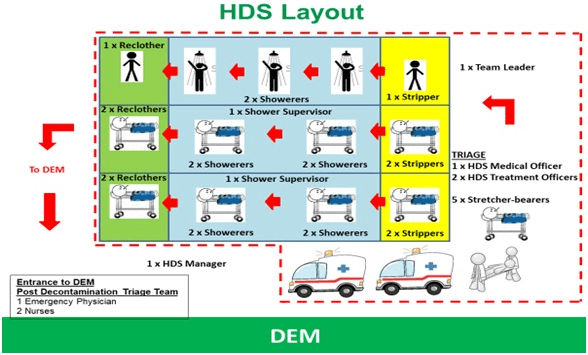
The rapidly deployable HDS has capability to decontaminate 42 casualties per hour including 24 non-ambulatory and 18 ambulatory casualties, hence increasing the decontamination capabilities of SGH compared to the commercial decontamination station located off site from the ED which had capability to decontaminate 36 casualties per hour including 6 non-ambulatory and 30 ambulatory casualties. The layout of the HDS is as shown in Figure 3 with 1 ambulatory and 2 trolley shower lanes each divided into 3 enclosed sections beginning with disrobing, showering and re-clothing areas.
Figure 3. Layout of the Hospital Decontamination Station (HDS) Located just Outside of the Entrance to the Department of Emergency Medicine (DEM)
There are several unique features of the HDS that are illustrated below:
1. An innovative idea that maximizes use of limited space for dual functions of ambulance parking during daily routine operations and decontamination station during chemical disasters, while preserving aesthetics. There is no need for additional storage space as deployment screens and showers are stowed up on the ceiling with minimum maintenance required (Figures 1A, 1B and 1C).
2. Close proximity to ED, which operates round the clock and provides initial manpower to operate the system.
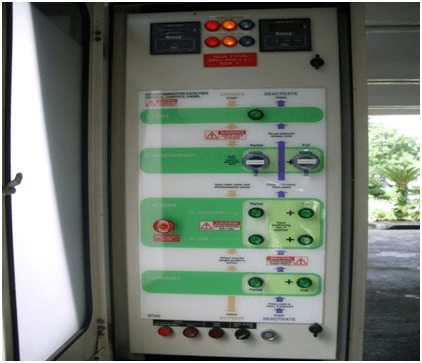
3. Rapid deployment (within 5-minutes of activation) by one staff member operating a control panel with clearly displayed instructions that are easy to follow (Figure 4).
Figure 4. Control panel for activation of Hospital Decontamination Station with Options for Partial or Full Deployment
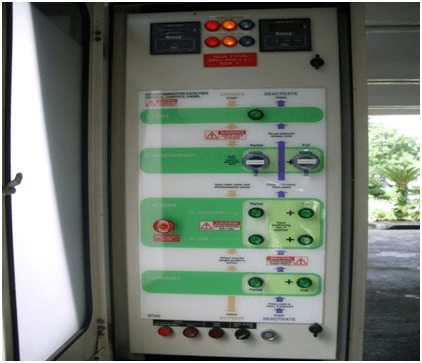
4. Scalable deployment (partial or full) according to caseload depending on small or large scale incident (i.e. the number of lanes deployed can be selected) giving better control over limited space.
5. The enclosed part of the HDS is separated into 3 sections, disrobing area for removal of contaminated clothing, shower section and drying and re-clothing section. This allows for privacy while casualties are undergoing decontamination.
6. Separate sections for ambulatory and non-ambulatory casualties with clear markings on the floor to indicate direction of casualty flow to facilitate work processes.
7. Self-contained disrobing, shower and re-clothing compartment formed by flexible longitudinal screens (premature ventricular contractions (PVC) coated polyester yarn with counterweights and anchors at base to prevent movement) and specially designed lateral cut up staggered screens ensuring ease of movement of casualties and staff working in the HDS.
8. Dedicated, self-contained ventilation system (exhaust fans) which suctions air from within the decontamination station, passing through filters before blowing out to the atmosphere facilitating cooling for staff working with protective suits and reducing contamination within the confined space of the HDS in an environmentally friendly manner.
9. In-built, showers spray heads and soap dispensers deployed from the ceiling to facilitate decontamination, maximize space utilization and ensure decontamination crew safety (Figure 5) by reducing clutter and obstacles which predisposes to fall hazards.
Figure 5. View from the Trolley Shower Lane within the Hospital Decontamination Station (HDS) Showing Water Hose Deployed from the Ceiling upon Activation

10. A large holding tank located beneath the HDS to contain the decontamination effluents for subsequent analysis and testing to determine safety for release into the sewerage system ensures water pollution control. This serves to conserve the environment.
Utility of the Hospital Decontamination Station (HDS)
Since its construction, the HDS has been used for several chemical incidents involving industrial chemical contaminated casualties and accidental toxic release situations.5-7 The rapid deployment capability allowed the incidents to be promptly managed preventing escalation of the incident with good outcomes.
The HDS has also been deployed successfully many times a year for both routine training as well as hospital and national disaster preparedness exercises (Table 1).
| Table 1. Hospital Decontamination Station (HDS) Utilization Over the Years |
| Year |
HDS Training Courses |
HDS Chemical Disaster Exercises |
| 2012 |
8 |
1 |
| 2013 |
6 |
1 |
| 2014 |
10 |
1 |
| 2015 |
11 |
– |
| 2016 |
13 |
2 |
| 2017 |
18 |
2 |
| 2018 |
23 |
2 |
DISCUSSION
A significant difference between hazardous materials incidents (chemical disasters) and conventional disasters involve the presence of chemical contamination in the environment as well as on casualties arriving from the incident site. This predisposes to ongoing chemical toxicity to the casualty as well as poses added risk to the rescuers and healthcare personnel dealing with such contaminated casualties.
In the Sarin incident in Tokyo in 1995, it was noted that approximately 9.9% of rescue workers2 (emergency medical technicians (EMT’)) and 23% of hospital staff3 dealing with these chemical contaminated casualties suffered from symptoms due to secondary exposure from chemicals off gassing from clothing’s of the casualties. Similar problems with secondary exposures amongst rescue personnel and hospital staff was noted in a similar attack4 involving Sarin in Matsumoto, Japan in 1994. It is noteworthy that no field or hospital decontamination of casualties was done in both these incidents.
Our own local experience,5,6,7 from treating casualties arriving from accidental toxic exposure has reinforced the potential risk of secondary exposure of healthcare workers from hazardous materials and has demonstrated the benefits of timely decontamination.
Hence, in chemical disasters it is of paramount importance to decontaminate all casualties so as to reduce the toxic effects on the casualty as well as to decrease the risk of secondary transmission. The latter is important to reduce the escalation of the event by spread of contamination and to reduce the loss of limited rescue and healthcare resources at a time of increased demand in a disaster situations.11 The basis for this has been recognized and there is guidance from occupational safety and health administration (OSHA)12 on best practices to follow in such situations. SGH has adapted and evolved its hazardous materials response contingency plans over time incorporating specific decontamination protocols into their disaster response plans13 (Figure 6).
Figure 6. Decontamination Crew Showering Casualty in Shower Section

There are many recommendations for hospital-based decontamination.14,15,16,17,18,19,20 However, there is limited information on the specific infrastructure required and the necessary manpower and logistical support to execute a successful hospital-based decontamination system. There are many areas that need to be addressed for hospitals to be prepared to deal with hazardous materials mass casualty incidents21,22,23,24 and it is hoped that by sharing our experience on the specifics of one of our crucial assets, others would be able to gain some insights into what it entails and what needs to be done to be ready when the need arises.
CONCLUSION
The HDS marks an important milestone in the hospital’s preparedness in dealing with hazardous materials disaster management. It is expected to be the primary decontamination facility for contaminated casualties from the incident site who make their way promptly to the hospitals ED bypassing onsite decontamination. With ED and hospital staff trained in deployment and operations of the HDS it will no doubt be an important countermeasure in the armamentarium for managing contaminated casualties and in the hospital’s hazardous materials incident contingency response plans for many more years to come.
ACKNOWLEDGEMENTS
Figures presented in this article belong to the author.