INTRODUCTION
Cystic fibrosis (CF) is the most common inherited life-shortening disease among White populations. It affects multiple organ systems, primarily the lungs and pancreas, and results in premature death due to respiratory failure.1 There has been a dramatic increase in the life expectancy of CF patients over the last decade, and median survival increased from 31.3 years in 2002 to 41.1 years in 2013.2 This increase has been largely attributed to better CF care, involving multiple regimens and treatment in designated CF centers. However, the treatment is complex and usually takes several hours a day. It involves several oral and nebulized medications, nutritional support and airway clearance therapy.3
Poor adherence to the treatment regimen may lead to increased morbidity and mortality, reduced quality of life and higher health care costs.4 Rates of adherence for chest physiotherapy have been estimated to be 40-47%, and much lower for dietary recommendations (16-20%).5
Adherence to the treatment regimen may be influenced by knowledge about the disease and the therapeutic regimen, by patient-provider communication and by regimen characteristics.5 It may also be influenced by the patient’s socioeconomic background, culture, religious beliefs and his own beliefs, which encompass illness perception.6,7 In 1984, Leventhal, et al. presented the self-regulatory model of health and illness; according to this model, patients construct their own representations, thus helping them with their coping responses.8 Based on this model, an illness perception questionnaire was developed.
In Israel, there are significant differences between Jews and Arabs in terms of socioeconomic status, sanitary conditions, educational level and the attitude toward child healthcare. The Arab population (Muslims, Christians and Druze) is a minority, consisting of 25% of the general population. Most reside in special villages or are segregated in special neighbourhoods in the city. They are surrounded by extended families and carry a high burden of care for the sick, disabled and elderly. The lower socioeconomic status is strongly associated with poorer health. Moreover, high rates of consanguineous marriages and the refusal to perform prenatal diagnosis contribute to a higher rate of genetic diseases in the Arab population.9
The CF center at Ruth Rappaport Children’s Hospital takes care of 80 patients, 60% of whom are Israeli Arabs. Their different cultural and religious background may influence their knowledge about CF, the strength of familial support, the sense of control and the confidence with the medical system, hence influencing their illness perception. Studies have emphasized the need for ‘cultural suiting’ of medical services when dealing with patients from different cultures.10,11
The aim of our study was to examine the cultural differences in illness perception and/or treatment adherence, and the possible associations between them.
METHODS
Participants
This was a cross-sectional, single center pilot study. CF patients aged >12 years were recruited during a routine clinic visit. The study was approved by the institutional review board. Patients or their legal guardian received an explanation and signed an informed consent. Demographic data was recorded. The patients were considered as Jews or Arabs (Muslims, Christians or Druze).
Procedures
Clinical characteristics, such as illness duration, Body Mass Index (BMI) and Forced Expiratory Volume in the 1st second (FEV1), were collected from the patients’ files. Illness severity was calculated using the validated CF-ABLE score. This score assesses severity and predicts outcome in CF patients.12
Each patient was interviewed by a psychologist in his own native language and completed illness perception questionnaire (based on Leventhal’s model). The revised questionnaire (IPQ-R) contains 70 items;8 the illness perception (belief about illness) incorporates the following nine components: identity (the nature of the disease), time-line (acute/chronic), consequences (the effect of the disease on the patient’s life), personal control (how much the patient controls the disease), treatment control (how much the treatment affects the disease), illness coherence (how much the patient understands his disease), time-line cyclical (how much the disease is predictable and stable), emotional representations (the emotional effect of the disease), causes (what the patient believes causes his disease).
With the exception of the identity subscale, responses are rated on a 5-point scale, ranging from 1 (strongly disagree) to 5 (strongly agree). The identity scale consists of 12 commonly experienced symptoms on a nominal scale (yes/no). The patients are asked if they experience each symptom and if they believe it is related to their illness. After reverse scoring appropriate items, a score for each subscale is obtained.8,13
Evaluation of adherence to the prescribed treatment regimen was performed using a self-report questionnaire, taken from the CF My Way program. The patient’s self-report of type and frequency of medication use was compared to the physician’s orders on the previous visit.
STATISTICAL ANALYSIS
Statistical analysis was performed using SPSS-18.Spearman’s rho correlation was used to determine the relationship between each of the nine statements and adherence to treatment and between illness perception and illness severity score. Marginal Homogeneity Test was used to compare self-reported treatment with the doctor’s orders. P<0.05 was considered as statistically significant.
RESULTS
Participants
Of 80 CF patients, 55 were older than 12 years of age; 35 Arabs (17 males) and 20 Jews (15 males). Thirty-three patients, 10 Jews and 23 Arabs, agreed to participate in the study. Their demographic characteristics are presented in Table 1, and reflect the demographic distribution in our clinic. There was no significant difference in age, illness duration, BMI, FEV1 and illness severity between the groups. The group of Jewish patients compromised of mainly males (9/10), with marginal statistical difference (p=0.05).
| Table 1: Demographic characteristic of patients. |
|
Jews (N=10) |
Non-Jews (N=23) |
P value |
| Age |
23.1±9.8 |
23.6±9.1 |
0.82 |
| Gender (% male) |
9(90) |
11(48) |
0.05 |
| Illness duration (years) |
18.9±8.5 |
17.3±6.2 |
0.95 |
| BMI (kg/m2) |
20.0±3.2 |
22.7±4.2 |
0.07 |
| FEV1 (% predicted) |
70.6±28.6 |
62.5±21.5 |
0.38 |
| Illness severitya |
2.0±1.7 |
2.7±2.5 |
0.66 |
Values are presented as mean±SD.
aIllness severity presented as CF-ABLE score |
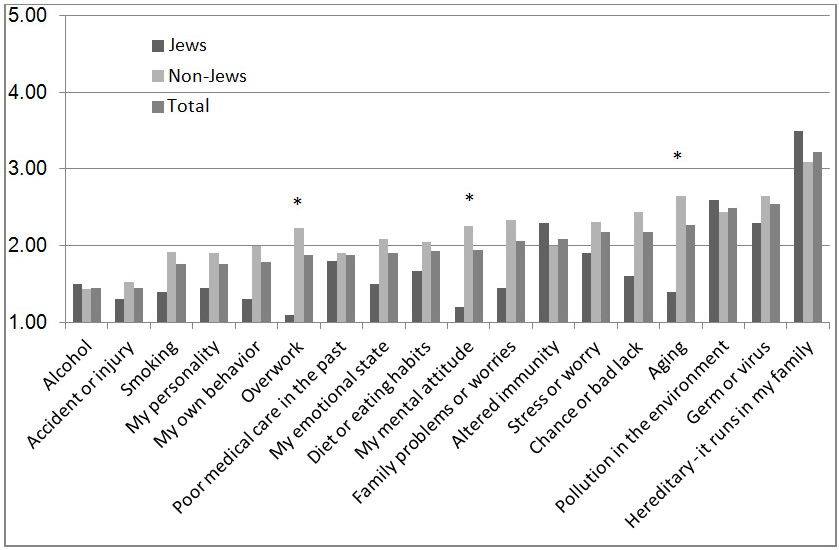
Illness Perception
In the identity scale, weight loss, fatigue and upset stomach were the most frequent symptoms endorsed by the patients (85%, 76% and 73%, respectively – data not shown), whereas breathlessness and weight loss were most frequently attributed to CF (87% and 77%, respectively). The scorings of seven out of nine illness perception subscales are presented in Table 2. There was a significant difference in the time-line cyclical score (8.8±2.8 vs. 12.6±3.1 for Jews and Arabs, respectively; p=0.002). The time-line score was higher in Jews, approaching statistical significance (26.5±5.8 for Jews and 22.4±5 for Arabs; p=0.055). When analyzing the correlation between the illness perception and the illness severity score, there was a significant correlation between treatment control and illness severity scores (r=0.41, p=0.049) in the group of the Arabs. No correlations were found in the group of Jews or for the other illness perception subscales. The results of the cause scale are presented in Figure 1. The patients endorsed most strongly “hereditary – it runs in my family” as a cause for their disease, with “alcohol” and “accident or injury” being the least favored attribution. “Pollution” and “germ or viruses” were also commonly endorsed. There was a significant difference between Jews and Arabs regarding the causes “overwork”, “my mental attitude” and “aging”, being less endorsed by the Jews.
| Table 2: Illness perception subscales scores. Identity scale not presented; causes scale presented in Figure 1. |
| Scale |
Jews |
Non-Jews |
P value |
| Time-line |
26.5±5.9
28.5(11-30)
|
22.5±5.1
23(10-30) |
0.055 |
| Consequences |
16±2.7
15(13-21)
|
17.7±2.5
17(14-23) |
0.085 |
| Personal control |
15.8±3.5
15(11-21)
|
17.1±3
16(11-26) |
0.27 |
| Treatment control |
18.7±5.4
20(5-24)
|
20.3±2.9
20(13-25) |
0.29 |
| Illness coherence |
20.2±4.9
22.5(13-25)
|
20.2±4.1
21(11-25) |
0.98 |
| Timeline cyclical |
8.8±2.9
9.5(4-13)
|
12.7±3.2
13(5-20) |
0.002a |
| Emotional representation |
14.7±9.1
11.5(6-28)
|
16.9±6.5
16(6-30) |
0.44 |
Values are presented as mean±SD and median (range).
astatistical significance. |
Figure 1: Causes of the Disease – Mean of Answers of Jews, Non-Jews and Total Group are Presented
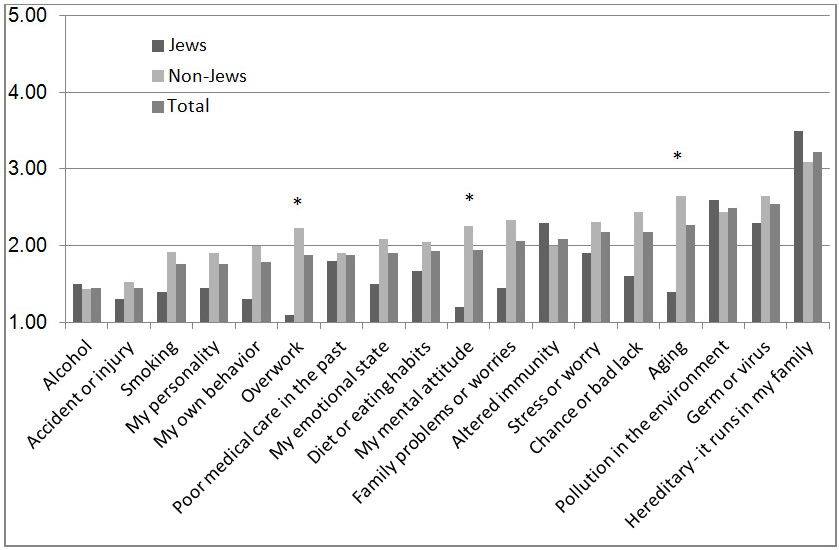
*statistical difference between Jews and non-Jews.
Treatment Adherence
The results of the patient’s self-report, the physician’s recommendations and the comparison between them are shown in Table 3. Chest physiotherapy and inhaled antibiotics were performed significantly less than recommended (p<0.001 and p=0.036, respectively). However, there was full concordance between patient’s reports and doctor’s recommendations regarding creon (p=1). Only five patients injected insulin with full concordance with the doctor’s order (p=1; data not shown). When analyzing Jews and Arabs separately, the difference regarding physiotherapy remained significant (p=0.02 for Jews, 0.003 for Arabs), whereas the difference regarding inhaled antibiotics became non-significant.
| Table 3: Treatment adherence – patients’ self-reports and physician’s recommendations. |
| P value |
Physician’s
recommendation |
Patient’s report |
Type of treatment |
| <0.001a |
4.5±0.8
4(3-6) |
3.2±1.5
4(1-6)
|
Physiotherapy
N=31
|
| 0.59 |
3.4±1.9
4(1-6) |
3.1±2.2
1(1-6)
|
Bronchodilators
N=25
|
| 0.27 |
3.07±2
4(1-6) |
2.6±2
1(1-6)
|
Hypertonic saline
N=27
|
| 0.18 |
4±.000
4(4-4) |
3.7±1.1
4(1-6)
|
Pulmozyme
N=32
|
| 0.29 |
3.9±1.8
5(1-5) |
3.6±1.8
5(1-6)
|
ICSb
N=29
|
| 1.00 |
3.1±3
6(1-6) |
3.1±3
6(1-6)
|
Pancreatic enzymes
N=25
|
| 0.06 |
3±1.4
4(1-5) |
3.5±1.5
4(1-6)
|
Vitamins
N=29
|
| 0.5 |
2.4±1.1
3(1-6) |
2.3±1.5
2(1-6)
|
Oral antibiotics
N=25
|
| 0.036a |
3.6±1.9
5(1-5) |
3±1.9
4(1-5)
|
Inhaled antibiotics
N=26
|
| 0.79 |
3.1±0.3
3(3-4) |
3±1.6
4(1-6)
|
Physical activity
N=27
|
Values are presented as mean±SD and median (range).
astatistical significance
bICS=inhaled corticosteroids |
Illness Perception and Treatment Adherence
A correlation analysis was used to determine the relationship between each of the nine illness perception subscales and adherence with treatment for the whole group (33 patients). A difference between the physician’s recommendation and the reported treatment was defined as low adherence, while identical recommendations and reported treatment was defined as good adherence. There was a statistical difference between time-line score and good adherence for hypertonic saline (p=0.039), and between illness coherence score and adherence with bronchodilator use (p=0.037). The correlation between consequences score and use of inhaled antibiotics approached statistical significance (p=0.054). There were no significant correlations between the other subscales and adherence.
DISCUSSION
In this study, we evaluated the differences in illness perception, treatment adherence and the association between them in Jewish and Arab CF patients treated in our center. The diversity of our population (reflecting the diversity of the Israeli population) enabled us to examine patients treated by the same doctors. Patients were divided into two groups, Jews and Arabs, with similar demographic variables but different religious and cultural backgrounds.
Previous studies supported the relationship between the components of illness representation described by Leventhal and a range of psychological outcomes, including coping, functional adaptation and adherence to treatment.8 Addressing illness perception early on with patients may provide an opportunity to improve the concordance between doctor and patient beliefs, to decrease the patient’s anxiety and to improve his understanding of the information provided.14
The analysis of the illness perception scores highlighted several points. In the illness identity analysis, most patients had gastrointestinal symptoms, but did not attribute them to CF; while respiratory symptoms and weight loss were attributed to CF. Since CF centers around the world are a part of Pulmonary Services, the respiratory aspects of the disease may be more emphasized.
Two illness perception scales showed differences between Jews and Arabs. The time-line score was higher in Jews, whereas the timeline-cyclical score was higher in Arabs. Thus, the Jewish patients considered their disease as prolonged and chronic, while the Arabic patients viewed the disease as more fluctuant and less predictable. When correlating illness perception with illness severity (based on CF-ABLE score), the only significant correlation was between illness severity and treatment control in the Arab patients. This finding may have implications when addressing adherence issues in these patients. Although Arab patients considered their CF as cyclic and non-predictable, in severe disease they tended to believe that treatment can control their disease. This may be explained by the immediate relief brought by intensive treatment. We are not aware of previous studies comparing illness severity and illness perception in different cultural backgrounds.
When analyzing the cause subscale, there were misconceptions about the causes of CF, with significant differences between the groups. Although it is a genetic disease, only about half the patients endorsed “hereditary” as a cause. All families received repeated explanations regarding the hereditary nature of the disease; this misunderstanding probably reflects the tendency of some families to withhold this information from their children.
Air-pollution and germ or viruses were endorsed as important causes. Viral or bacterial agents are the main cause for pulmonary exacerbations in CF patients. This suggests misinterpreting the question as a cause of exacerbations and not a cause of disease and may support the concept of the cyclical nature of the disease by some patients. In three causal domains, there was a significant difference between Jews and Arabs. Arabs felt that overwork, mental attitude and aging are causes for CF exacerbations. Baron-Epel, et al.15 analyzed the pattern of utilization of health services among Jews and Arabs in Israel. There was a different pattern, with Arabs using less specialist care, more family physician care and higher rates of hospitalizations. The differences were attributed to their rural way of life, and to differences in culture, norms and behaviour. Despite more negative health outcomes in the Arab population, they perceived their health as better and reported less chronic diseases.15 Quittner, et al. found that racial or ethnic minority was related to worse social and emotional functioning and more severe consequences of the disease.16
The analysis of self-reported treatment and comparison with the physician’s prescription yielded several findings. We found significant low adherence to chest physiotherapy and inhaled antibiotics, as opposed to perfect adherence to pancreatic enzymes (similar in both groups). The immediate clinical effect of poor adherence to pancreatic enzymes and the relative easiness and short time of the procedure may explain this difference.
There is evidence of low adherence to long-term preventive treatments in other chronic diseases.6 In CF, adherence varied by treatment component and measurement method, but overall rates of adherence were below 50%.17 DeLambo, et al. found that a more positive family relationship was associated with better adherence to airway clearance and aerolized medications, but not to other treatment regimens.18 Recently, Grossoehme et al. found that certain forms of parental spiritual/religious beliefs and coping styles, are associated with treatment adherence.19
When analyzing correlations between illness perception and treatment adherence, there was a correlation between some aspects of illness perception and inhaled therapies. Those who understood the disease better (higher illness coherence), those who believed the disease was chronic (higher time-line), and those who felt the disease has a substantial effect on their lives (higher consequences) had better adherence for certain aspects of inhaled therapies. Illness coherence represents how the illness “makes sense” to the patient, and may play an important role in long-term adjustments and response to symptoms.8
In other chronic diseases, there is evidence that perceived illness severity predicts adherence to treatment. Reasons for non-adherence were busy schedule, forgetfulness, but also “my disease is not so serious” and “I feel well without treatment”.6
Several studies examined the correlations between illness perception or severity and adherence in CF patients. High perceived severity may lead to avoidance or denial6 in some patients, but to increased adherence in others.18 Bucks et al. found that time-line and treatment control scores correlated with adherence to antibiotics.1
Interventions to improve adherence have been largely studied. A Cochrane analysis found that CF pediatric patients who received nutritional intervention plus behavioral management training consumed more calories per day than children just receiving the nutritional intervention. They also found that a structured decision-making tool for adults considering lung transplantation improved their knowledge, assisted in setting realistic expectations, and reduced indecision.20 Moore, et al. examined an intervention program for CF patients and their clinicians. Educating clinicians about prescribing guidelines, providing feedback on adherence and monitoring prescribing patterns over time improved adherence. Mean FEV1 showed improvement after several months of sustained adherence and trended towards statistical significance.21
There are few interventions developed to change illness perceptions. One notable example is the trial of a psychological family-based intervention to change illness perceptions in patients with poorly controlled type 2 diabetes. The intervention group showed a significant change in illness perceptions and improvement in Glycated hemoglobin (HbA1C).22
The main limitation of our study is the small number of patients, especially in the Jewish group. Treatment adherence was self-reported and was not measured. There may be over reporting of self-administered medications compared with pill counting and blood or urine analysis.6,17 Another limitation is the gender difference; with 90% of Jewish group are males. This may also affect illness perception and treatment adherence. More patients and balanced gender should be considered.
In conclusion, illness perception may be affected by cultural background and in turn, may influence treatment adherence. Adherence interventions should be culture-sensitive; they should focus on providing education to improve knowledge and skills to conduct the therapy. Identifying illness perceptions may help solving barriers to adherence, and matching the type of therapy to the patients and their families. Further multi-center studies are needed, which may delineate the different cultural effects on illness perception and measured treatment adherence.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
ACKNOWLEDGEMENTS
The authors acknowledge the statistical help of Mrs. R. Leiba from the Medical Statistics Unit, Rambam Health Care Campus. The study was supported by an investigator-initiated grant from Novartis.