CASE REPORT
A 42-year-old diabetic male was admitted in our Intensive Care Unit (ICU), a follow-up case of bilateral renal-calculus, who underwent left sided percutaneous nephrolithotomy (PCNL) in some peripheral hospital. There was alleged history of massive bleeding (about 4.5 liters) intra-operatively owing to injury to renal parenchyma. There was documented placement of double J stent and renal parenchymal laceration repair. Patient had received four units of packed cell volume during intra-operative period. He was shifted to the ICU, intubated requiring high vasopressor support, oliguria and high total leucocyte count (TLC) 38,000/mm3. All his routine investigations with cultures were sent, and he was empirically started on Tecoplanin, Meropenem, metronidazole, in order to contain infection. Inotropic support could be tapered owing to adequacy of fluids, and blood products. Patient responded to antibiotics with falling trends of TLC over 5 days. Culture reports obtained from blood, trachea and urine were sterile but that of abdominal drain was suggestive of Acenitobacter, sensitive to colistin and levofloxacin, same were added on day five. His blood sugars were controlled on sliding scale of insulin. Patient was doing well, but had persistent spikes of fever despite antibiotic coverage. Patient required pressure supported breaths but could not be extubated owing to altered sensorium and drowsiness, although his non-contrast computed tomography (NCCT) head was within normal limits. Upon repeating cultures on day 10, no growth of organism was found. Enteral feeding could not be initiated owing to persistent high aspirate from Ryle tube, 1.5-2.5 liters daily. Total parenteral nutrition neutralized with 16 units insulin was started initially, but owing to high blood sugars, was later neutralized with 30 units of insulin. Patient was tracheostomisedon day 14 owing to need for prolonged ventilation and we could wean off our patient to T-piece. On day 16, cultures obtained from blood, trachea and urine were suggestive of a fresh crop of infection. The organism identified was Providencia stuartii, which was resistant to all the available antibiotics (Table 1). Procalcitonin levels were very high and were suggestive of high risk of sepsis and septic shock (Table 2). Tazact, ceftriaxone and vancomycin were added empirically as patient had received meropenem and colistin but still his fever remained between 102-105 ○F. His urinary catheter, tracheostomy tube and central line were changed subsequently in order to contain infection but patient continued to have tachypnea, fever, tachycardia, hypotension, unresponsive to fluids with oliguria and presence of purple urine. Patient had sudden deterioration over few days leading to full ventilator support requiring high dosage of vasopressor support. His chest X-ray were suggestive of bilateral acute respiratory distress syndrome, requiring very high fraction of oxygen (Figure 1). His vital organs gradually stopped functioning and ultimately we lost our patient after a course of 28 days in intensive care unit (ICU) (Figure 2).
| Table 1. Antibiotic Sensitivity Report from a Standard Laboratory |
| ORGANISM-Providencia Stuartii |
ANTIBIOTIC SENSTIVITY
(as obtained from tracheal/urine/blood culture) |
| Extended beta lactamases |
Positive |
| Carbapenamases |
Positive |
|
Group A (First line)
Ampicillin
Gentamycin
Cefazolin
Tobramycin
|
Resistant
Resistant
Resistant
Resistant
|
|
Group B (second generation)
Amikacin
Amox-clavulunic acid
Ampicillin-sulbactum
Piperracilin-tazobactum
Ticarracilin-caluvulanate
Cefuroxime
Cefipime
Cefotaxin
Ceftriaxone
Ciprofloxacin
Levofloxacin
Dorepenem
Impipenem
Meropenem
Irtapenem
|
Resistant
Resistant
Resistant
Resistant
Resistant
Resistant
Resistant
Resistant
Resistant
Resistant
Resistant
Resistant
Resistant
Resistant
Resistant |
|
GROUP C (third line)
Azetronam
Ceftazidime
Tetracycline
Tigecyclin
|
Resistant
Resistant
Resistant
Resistant |
|
Group O (not routinely tested or approved by FDA/CLSI
Colisitin
Trimethoprim-sulphamethaxaozole
|
Resistant
Resistant
|
| Table 2. Serum Procalcitonin Levels (Marker of Sepsis) |
| Procalcitonin |
24.55 ng/ml |
|
Reference Range (ng/ml)
<0.5
0.5-2
>2
|
Low Risk of sepsis/septic shock
Borderline risk of sepsis/septic shock
High Risk of sepsis/septic shock
|
Figure 1. Specific Note Can be Made of Change in Color of Urine, Suggestive of Pus and Pinkish Purple Hue in Tubing’s and Uroflowmeter, and Simultaneously Urine Culture Suggested of Growth of Providencia Organism

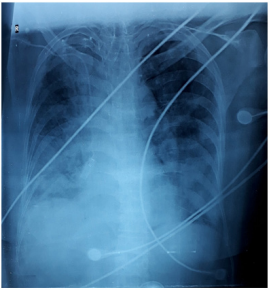
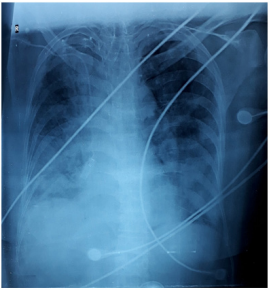
Figure 2. Bed Side Chest X Ray is Suggestive of Bilateral Infiltrates in Middle and Lower Zones with Blunting of Bilateral Cardio-Phrenic Angles
DISCUSSION
Sepsis is defined as life threatening organ dysfunction caused by dysregulated host response to infection.1 Providencia is a class of enterobacteriaceae family, with 8 recognized species and P. stuartii is the most frequent. It is commonly found in soil, water and sewage, but is a notorious opportunistic pathogen in patients who have long-term indwelling urinary catheters, diabetics, immunocompromised or severe burns. The most common source of sepsis is via urinary route as P. stuartii adheres directly to the urinary catheters, and adheres to uroepithelial cells via fimbriae. Godebo et al2 suggested that 75% of Providencia isolates were multidrug resistant and Linhares et al3 identified Providencia species as the most common cause of multi drug resistant urinary tract infection. Over 90% of isolates were resistant to aminoglycosides, cephalosporins, 20% to other penicillins, quinolones, sulphonamides. Ten percent were resistant to II-III generation cephalosporins and 5% to aztreonam.
Carbapenems (Imipenem and Meropenem) are considered as the best choice for empirical therapy in life threatening outbreaks caused by P. stuartii, but our patient did not respond to all of these. Amikacin and beta lactamase inhibitors such as piperacillin/tazobactum are preferred in non-life threatening infections.
There were various factors which could have resulted in the nososcomial infection of P. stuartii in our patient. Our patient had alleged history of injury to renal parenchyma during his percutaneous nephrolithotomy (PCNL) procedure, initial drain culture sensitivity was suggestive of acenitobacter which was sensitive to colistin. He initially responded to three day course of the same, but owing to surge of pyrexial episode, we extended the course of colistin for further 5 days. Hayakawa et al4 suggested increased use of colistin can be associated with increase in infection of P. struatii. Surgical drains were subsequently removed, but the drain source could have resulted in Providencia infection. Secondly he had catheter in situ which could have been a nidus of infection. Thirdly, knowing that he was diabetic, provision of nutritional requirement by total parenteral nutrition led to persistently high blood sugar and required high dose of insulin infusion. Because of strong association of providencia urinary tract infection with chronic urinary catheterization, removal and change of the same was done. Prevention is the best cure in dealing with these organisms, as far as possible. Urinary catheters, drains, tracheostomy tubes in chronic debilitated patients especially who are diabetics or immunocompromised, should be changed contrary to the norms.
Latest Guidelines for Prevention of Catheter-Associated Urinary Tract Infections,5 recommend against changing indwelling catheters or drainage bags at routinely fixed intervals unless there are clinical indicators like infection, obstruction or when closed system is compromised, seems questionable in our case. Considering this scenario, changing the catheter every 15 days should be undertaken in patients who are chronically immunocompromised, diabetics especially with uncontrolled blood sugars and elderly. Control of blood sugars in the normal range should be a norm and as far as possible, blood glucose levels should be less than 180 mg/dL as suggested by sepsis guidelines in 2016.1 Enteral route should be preferred for nutrition except in circumstances such as in ours where parenteral is the only way left to provide nutrition.
This is yet another instance where the importance of preventive measures cannot be over emphasized. Chasing infection by escalating antibiotics or discovering newer ones seems to be rather futile. Hand hygiene and strict aseptic precautions are still of paramount importance and most effective standalone measures. Clinical guidelines may be best for patients overall but may be inappropriate for all individuals. Hence bedside clinical judgement still supersedes clinical guidelines.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.