INTRODUCTION
Ganglion cyst thought to be the result of myxoid degeneration of joint capsule and tendon sheath connective tissue.1 This lesion frequently origins from joint capsule, although may also originate from tendon sheath, muscle, nerve, and period. Hand-wrist, foot-ankle are the most common locations respectively.2 A study on knee magnetic resonance imaging (MRI) revealed 0.76% of the incidence of the peroneal ganglion cysts.3 Ganglion cysts are the typical lesions although peripheral nerve compression is rare. Peroneal ganglion cysts may lead neuropathy with pain, loss of sensation, weakness on six of the foot ankle and peroneal nerve palsy due to compression of the adjacent peroneal nerve.4 In this report, we demonstrate a tendon sheath originated peroneal ganglion cyst in large diameter at the proximal musculotendinous junction of peroneus longus muscle proceed to downward in muscle causes severe pain and loss of sensation on cruris.
CASE PRESENTATION
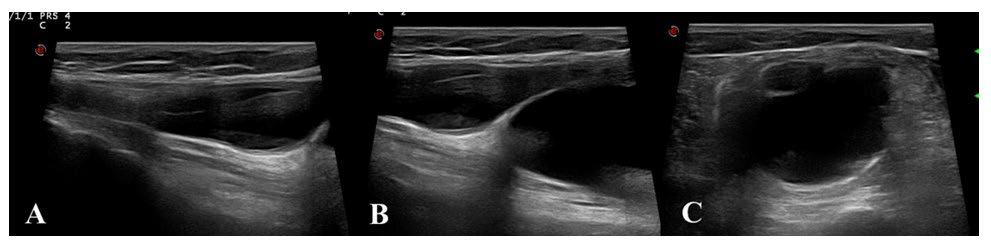
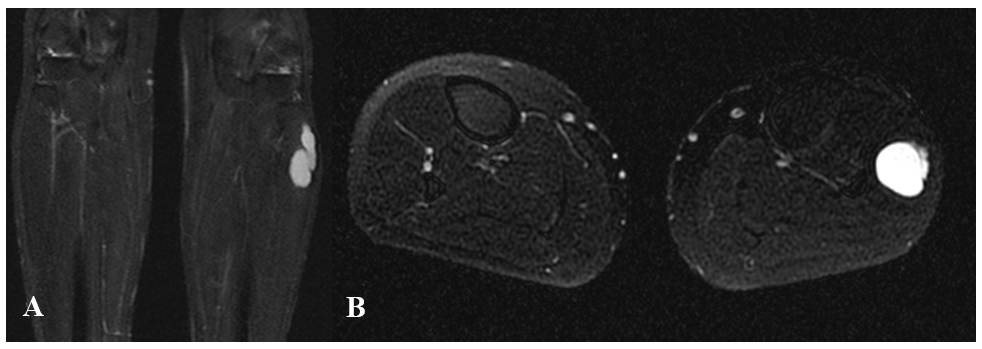
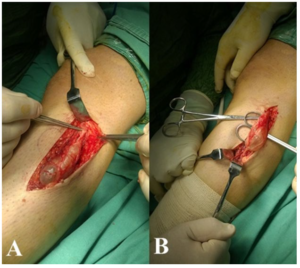
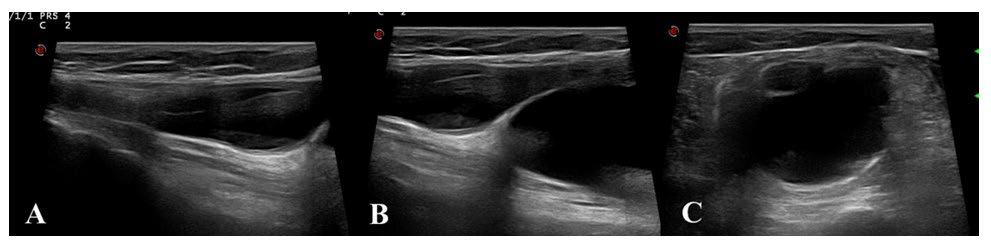
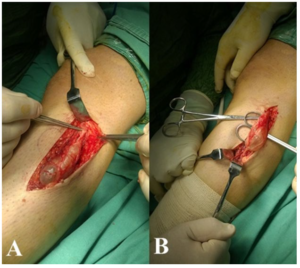
A 37-year-old man applied to a hospital with one-year progressive swelling on the lateral portion of left knee below and pain on the left foot back. In anamnesis, the pain was continuous in last 2 weeks. Physical examination revealed a large, rigid, immobile lesion in the pain location. The patient had loss of sensation on the anterolateral portion of the left cruris below. Ultrasound (US) imaging revealed an 8 cm in length and 3 cm in diameter at its widest point anechogenic cystic lesion spread with a narrow diameter from the left fibula head level to inferior (Figures 1A, 1B and 1C). MRI to characterize the lesion demonstrated an 83×35 mm lesion that was hypointense on T1- and hyperintense on T2-weighted imaging (Figures 2A and 2B). The lesion was originated from the peroneus longus tendon adjacent to lateral part of the left fibula; with a narrow diameter the lesion was proceeded to inferior and the diameter was increased. Preliminary diagnosis of ganglion cyst was held and diagnostic aspiration cytology applied to the patient. The material was serous and in gel consistency; the pathologic result reported as intense proteinaceous content. The patient underwent surgery with preliminary diagnosis of a ganglion cyst. Longitudinal incision applied on the lesion trace under the spinal anestesia. The lesion was reached between the musculus peroneus longus muscle fibers. The origin of the lesion observed as the tendinous component of the musculotendinous joint of peroneus longus muscle. The lesion dissected and total excisional biopsy was performed. The area washed with saline solution and after the bleeding control the wound location sutured (Figures 3A and 3B). The ganglion cyst diagnosis was proved by pathology examination. The patient had no pain or loss of sensation on the lateral portion of left lower leg after one month. There was no evidence of residue or recurrence on US imaging after 6 months.
Figures 1: (A and B) Sagittal section on the US. The cyst is forming with a narrow neck and spreads with widening in the muscle. (C) Axial section on US. The inferior component of the cyst demonstrates marked intramuscular trace.
Figures 2: T2-weighted coronal imaging (A) and T2-weighted axial imaging (B) demonstrate hyperintense cystic lesion in the peroneus longus muscle.
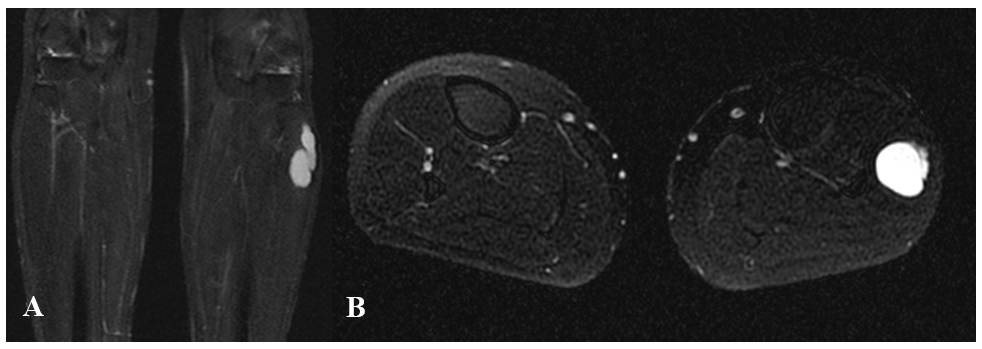
Figure 3: (A and B) Intraoperative appearance of the cyst.
DISCUSSION
Ganglion cysts mostly occur in hand-wrist and foot-angle, respectively.2 They may establish at any age, although peak incidence is in the thirties. It is more common in women than in men.5 Our patient was a 37-year-old man.
The exact etiology of the peroneal ganglion cyst is unclear, although trauma, synovial herniation, removal of synovial tissue during embryogenesis are mentioned.6 Our patient had no trauma history.
It is uncommon to have neurological symptoms due to impress of peroneal nerve and roots by a peroneal ganglion cyst, however, severe complications such as drop foot may also occur.3,7 Our patient had just sensation loss on left lower leg lateral portion without loss of strength. These cysts lead peroneal nerve compression may be peroneal nerve originated ganglion cysts and entitled peroneal intraneural ganglion cyst.7
Physical examination and diagnostic tools such as US and MRI may use in the diagnosis of a peroneal ganglion cyst. The US is useful because the technique is inexpensive, noninvasive and easy to implement. A ganglion cyst is a well defined anechogenic cystic lesion on the US. The US can distinct between the robust and cystic components of the lesion, although provides limited information about the relationship with surrounding tissues. The differentiation of ganglion cyst and cystic schwannoma is not always possible in the US. MRI is the selectable modality to determine the extent of the lesion.
A ganglion cyst is typically black on T1- and bright on T2-weighted images of MRI study. After the administration of intravenous (IV) gadolinium, the cyst wall may enhance mildly, although the center of the lesion is unenhanced.
In our patient, we applied US as a primary imaging technique and MRI in next step to demonstrate the relation of the lesion to peripheral structures. Our preliminary diagnosis was the ganglion cyst. Therefore we did not perform IV contrast material. We applied fine needle aspiration cytology for definitive diagnosis before surgery. The aspiration material was intense proteinaceous material on cytology. Histologically, ganglion cysts are filled with viscous gelatinous protein material consisting of hyaluronic acid, albumin, globulin and glucosamine.8
Synovial cyst, intramuscular myxoma, cystic degeneration of a schwannoma or neurofibroma, or synovial sarcoma are in the differential diagnosis.2
The recent treatment of peroneal ganglion cyst is marginal excision. Also, ligation of cystic peduncle or electrocoagulation has to be a part of surgery to avoid recurrence.7 In our patient, the peduncle was in large diameter. Therefore ligation or electrocoagulation was unrequired. After 6 months US control imaging demonstrated no evidence of recurrence.
Fine needle aspiration may be an alternative treatment choice in patients with ganglion cyst who hesitate from surgery.6,7
CONCLUSION
In conclusion, we aim to emphasize the ganglion cysts usually occur in hand-wrist and foot-ankle and may also establish in peroneal muscle. These cysts may cause peroneal neuropathy symptoms. US and MRI are the reliable tools in diagnosis.
CONFLICTS OF INTEREST
The authors declare that there are no conflicts of interest regarding the publication of this paper.
CONSENT
The authors have obtained oral consent from the patient for this article.
AUTHORS CONTRİBUTİONS
Özen Ö and Tosun A were involved in radiological imaging of this patient and writing of the case report. Aytekin K and Esenyel CZ were the orthopedic surgeons managing the patient.