INTRODUCTION
Schizophrenia (SZ) is a chronic mental disorder that affects about 1% of the world population, and mainly happens in the end of adolescence and the beginning of adulthood, regardless of gender or social groups.1 It is a disease characterized by distortions in thoughts, bizarre delusions and changes in sensory perception and inappropriate emotional responses that lead patients to some degree of deterioration.2
Its symptoms differ among individuals and may afflict them gradually or explosively. These symptoms are still divided into negative or positive. Negative symptoms of SZ, facing decreased brain function, were described by Kaiser et al3 as defining this condition, as it often manifests itself together, and differs from other psychopathological conditions.
Negative symptoms described were: apathy, loss of pleasures in activities once the provided, unwillingness to start a behavior directed at a goal and poverty of speech. As the positives symptoms are the level of mental disorders such as delusions, distortion of thoughts, unreal perceptions, such as audio-visual hallucinations, excessive anxiety, impulses and aggression.
The treatment of SZ, focused on minimizing the symptoms, is based on the use of antipsychotics. These drugs are inhibitors of psychomotor functions (in excitation and stirring conditions) and minimize psychotic symptoms, such as delusions and hallucinations. These drugs can be classified as typical or atypical.
The major typical antipsychotic drugs block only D2 receptors. The atypical antipsychotic drugs are associated to lower risks of extrapyramidal effects, not block D2 receptors only, but also other monoamines, such as the 5HT-2. These include: Clozapine, Olanzapine, Quetiapine and Respiridona.4
Clozapine is a reference atypical antipsychotic, having distinct characteristics of the medications available before its release, which showed effective in 30% to 60% of psychoses that do not respond to traditional drugs, and low incidence of adverse effects, becoming the main indication for refractory schizophrenia. Atypical offer several important advantages over typical, including its characteristics of low risk of extrapyramidal symptoms such as akathisia, dystonia, parkinsonism and tardive dyskinesia, improved cognition, reduced suicide and minor depression compared with typical antipsychotics at clinically relevant doses.5
The use of antipsychotics is an important component in the clinical treatment of patients with schizophrenia, but has been associated with metabolic abnormalities5 and also obesity, diabetes, dyslipidemia, metabolic syndrome and high mortality.6
Associated with pharmacological treatment, nutritional and psychological treatments are very important in the improvement of the condition of these patients.7 Obesity is a non-transmissible chronic disease, which presents itself not only as a scientific problem, but also as a public health problem. The modern lifestyle with a more westernized diet, associated with a decrease in physical activity, converges to the increase in worldwide obesity.8
According to World Health Organization (WHO), obesity is defined as an abnormal fat accumulation that may impair health.9 Body mass index (BMI) is an index which correlates weight and height (kg/m2), thereby obesity is classified as BMI≥30 kg/m2.
The World Health Organization (WHO) projected that in 2005 the world would have 1.6 billion people over the age of 15 overweight (Integrated Management of Childhood Illness (IMCI) ≥25 kg/m2) and 400 million obese (BMI≥30 kg/m2). The projection for 2015 is even more pessimistic: 2.3 billion people overweight and 700 million obese. These data indicate a 75% increase in obesity cases in 10 years.9
In 2010, the Brazilian Ministry of Health and the Brazilian Institute of Geography and Statistics (IBGE) released two large surveys of the numbers of overweight and obesity in Brazil, called “VIGITEL Brazil 2009: Risk and Protective Factors Surveillance for Chronic Diseases using Telephone Survey and Household Budget Survey 2008-2009 (POF)”.10
Studies showed an excess weight in 46.6% of the population, was higher among men (51.0%) than among women (42.3%). Already the POF (2008-2009) shows a steady increase of overweight and obesity in the population over 20 years of age over 35 years. Overweight nearly tripled among men, 18.5% in 1974-1975 to 50.1% in 2008-2009. In women, the increase was smaller: from 28.7% to 48%.9
Obesity is associated with a lower quality of life both in schizophrenic patients and the general population. This is due to eating disorders and metabolic disorders such as oxidative stress. These patients deserve greater attention in the management and intervention in weight.5
The objective of this study is to evaluate the association of obesity with the use of clozapine in schizophrenic patients, as explained above, there is an increasing prevalence of obesity in recent decades, which compromises the expectation and quality of life (QoL) of these patients.
MATERIALS AND METHODS
A review of the literature was conducted between 2004-2015 on obesity in schizophrenic patients with clozapine, and the association of this atypical antipsychotic with these conditions was the main target of this study.
This research used two databases: PubMed (MEDLINE) and Journal of Capes. The terms used in the search were: “Schizophrenia”, “Obesity”, “Clozapine” and “Weight gain”.
The selection of items was conducted by a researcher, taking into account the following inclusion criteria: English language, both sexes, retrospective study, patients aged over 20 years, the minimum clozapine use time of three months and sample size equal or higher than 50 individuals.
For the extraction of data from the articles was prepared a card (Table 1).
| Table 1: Data extraction form. |
| Data extraction form |
| Article Title: ________________________________________________
Design: ______________________________________________
Medication And Use Time: _______________________________________
Tracking Time: ___________________________________
Sex: ________________________________
Patient Age: ______________________
Parameters Used to Evaluate Obesity: ______________________
Sample Size: _______________________
Study Outcome: ________________________ |
RESULTS
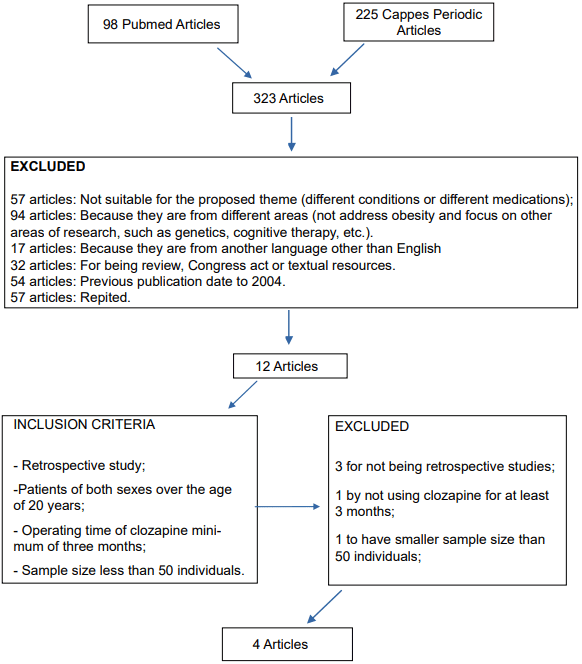
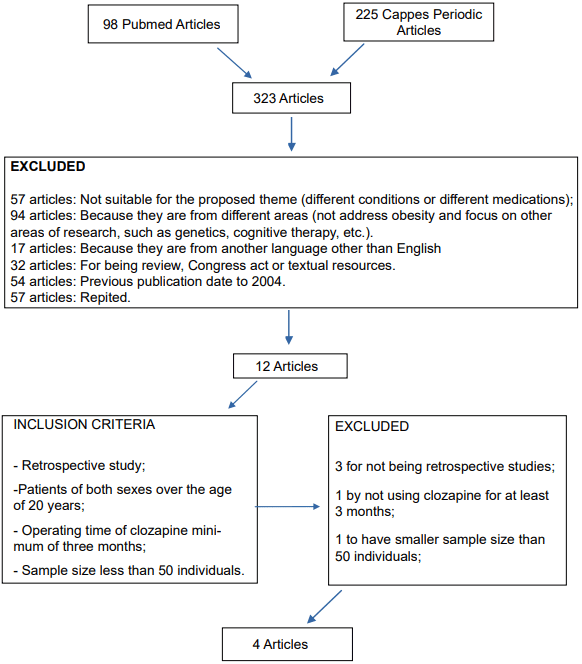
They were found 323 articles, of which 306 in English in the initial search. After careful selection, 57 were excluded because they did not conform to the proposed theme (different diseases or medications), 94 were excluded after reading the title because they are from different areas, 32 to be another type of resource, such as reviews or Congress act, 57 repeated, 54 previously published for 2004, the remaining 12 articles, which were read and examined again taking into account the inclusion criteria, with only 4 items selected and included in this review (Figure 1).
Figure 1: Organization chart of items excluded
Thus, the individual description of each study was made, following the reverse chronological order of publication as shown in Table 1 and their outcomes in Table 2.
| Table 2: Analysis of the articles included. |
| Analysis of the articles included |
|
Authors in studies
year
|
Outline |
Population
sample size |
Medication and time use |
Parameters used to evaluate obesity |
| Villanueva et al11
|
Coorte
retrospective study |
Men and women
76 patients |
Clozapine
18 to 56 weeks |
BMI*
and
body weight |
| Choong E et al12 |
Cross retrospective study |
Men and women
196 patients |
Clozapine, olanzapine, quetiapine, risperidone, lithium and valproate.
>3 months of use |
BMI*
and
body weight |
| Ya Mei Bai et al13
|
Retrospective study |
Men and women
96 patients, 55 being accompanied. |
Clozapine
8 years |
BMI*
and
body weight |
| Covell NH et al14 |
Retrospective study |
Men and women
38 patients |
Clozapine
2 years |
BMI*
and
body weight |
| *BMI: Body Mass Index |
The study Villanueva et al11 measured the change in BMI induced by clozapine, in both sexes, in two stages, 18 and 56 weeks follow-up. They analyzed 76 patients at 18 weeks and 57 in 56 weeks.
At first it was determined baseline BMI and then was made periodic reviews weight, height, BMI and clozapine dosage. As a result at 18 weeks of follow-up there was a variation in BMI of 1.83 kg/m2, and of these 18 patients (19.7%) had a decrease in BMI. There was no difference between sexes in BMI changes. At 56 weeks of follow-up there was a BMI range of 2.67 kg/m2, and of these 10 patients (17.5%) had a decrease in BMI. There was no difference between sexes in BMI changes, also this time. There was a statistically significant inverse relationship between BMI and baseline BMI in both times. In this study, the authors concluded that despite the increase in weight with the use of clozapine, physicians should not discourage the use for refractory patients.
Choong et al’s12 study evaluated the importance of side effects associated with weight gain psychotropic drugs and their metabolic consequences. Patients received for more than three months drugs: Clozapine, olanzapine, quetiapine, risperidone, lithium and/or valproate. 196 patients were analyzed. The weight gain (≥10% of initial body weight) after treatment with clozapine was reported in 47% of patients.
The prevalence of obesity (BMI≥30) was present in 38% of patients. The highest dose, an increase in appetite after the introduction of medication, type of medication (clozapine or olanzapine>quetiapine, or risperidone>lithium or valproate), and sex was significantly associated with the development of BMI.
Yamei Bai13 study tested whether the initial clozapine response is related to weight gain. This study was a retrospective study of 8 years of 96 hospitalized patients with schizophrenia. There was a loss of 41 patients (death, incomplete weights, unavailable medical records, change of antipsychotic). The monthly weight change data were analyzed, the initial clinical response, age, sex, clozapine, and concomitant use of mood stabilizers and other antipsychotics. To analyze the weight gain BMI was used.
The patients receiving clozapine (55 patients, 57.3%) throughout the study period, achieved an average weight gain of 11.7 kg (SD=1.6). The multiple linear regression analysis showed significant initial clinical response and lower initial body mass index was associated with higher weight gain. The results show that the initial response to the antipsychotic clozapine is associated with higher weight gain in the long term, measured over 8 years.
Covell NH14 study analyzed the percentage weight gain of 138 randomized patients taking clozapine for 2 years and 89 who continued to receive first-generation antipsychotics.
In each group, 39% of participants were women. Two patients who were randomized to clozapine, did not start its use and were excluded and 3 patients had their weight measured outside the patterns and were also excluded from the analysis
Table 2.
Demographic data were collected, the daily log of medications and weight from information available through chart review. When more than one weight measurement was available in a given month, we used the latest weight for analysis. It also calculated body mass index.
The groups did not differ significantly from the initial weight and average BMI. The random regression analysis showed that patients who switched to clozapine gained more weight than patients who remained in the first generation of anti-psychotic agents.
DISCUSSION
In the four studies selected in this systematic review, BMI was used as a parameter to assess weight gain. However, this parameter measures the weight as a whole, and does not assess body composition. Thus, the weight increase may be associated with increased lean body mass or fat mass, and only the latter being associated with obesity.
According Garn and colleagues16 there are three limitations to the use of BMI: The correlation with height, the correlation with the fat-free mass and the influence of body proportionality (size ratio of the legs/trunk), such that individual less leg length have a higher BMI. These limitations could jeopardize the use of BMI as body fat indicator.
To get a real idea of the incidence of obesity in these studies, the authors should associate with BMI, bioimpedance test or skin folds (done with skinfold), and then perform the comparison of these parameters before and after the use of clozapine Table 3.
| Table 3: Analysis of outcomes. |
| Analysis of outcomes |
|
Studies and authors
|
Outcomes
|
| Villanueva et al11
|
There was a change in BMI in both periods. In the 18th week this change was 1.83 kg/m2 and in the 56th week of 2.67 kg/m2. Only 18 patients (19.7%) had decreased BMI at 1 time and 10 patients (17.5%) had decreased this index in the 2nd time. There were no gender differences in observed changes in BMI. |
| Choong E et al12
|
The weight gain was reported in 47% of patients, greater than or equal to 10% of their initial weight. The prevalence of obesity (BMI≥30 kg/m2) was present in 38% of patients and clozapine or olanzapine were the drugs had a greater increase in appetite. |
| Ya Mei Bai et al13 |
The patients (55 patients – 57.3% of the sample) received clozapine throughout duration of the study, 8 years, increased on average 11.7 kg body weight. |
| Covell NH et al14 |
Patients who used clozapine had higher weight gain (13.7%) of those taking medications 1st generation (5.4%). Patients with normal weight were more likely to become obese (BMI≥30 kg/m2), especially among women. |
| *BMI: Body Mass Index |
To Cerve,16 although BMI has high correlation with body mass, it has low with height, so it is important to correlate with other independent measures of body composition, which determine the composition in terms of body fat and muscle mass to have greater reliability as anthropometric parameters, such as bioelectrical impedance, skinfold thickness, waist/hip ratio (WHR) and waist circumference (WC).
And the study of Choong,12 comparison was made with other antipsychotic drugs, and the results showed that clozapine and olanzapine are those with largest increase of appetite and consequent increased weight gain.
Studies show a high prevalence of obesity, hyperglycemia, dyslipidemia and metabolic syndrome in patients treated with atypical antipsychotics, with evidence of greater effect for those using clozapine and olanzapine.6
Like clozapine, olanzapine is also associated with weight gain, an increase from baseline of 6.12 kg in 6 to 12 months of treatment.17
In the study Covell14 significant difference in weight gain after Clozapine especially in women, unlike other studies. This may have been because it was a study with the smaller sample size of the four selected. In the other there was no difference between the sexes in both studied moments.
The databases used periodicals and CAPES, PUBMED is quite academic relevance, encompassing medical articles from various fields, which increases the credibility of the review further.
CONCLUSION
In all items selected for this study, obesity was associated with clozapine. However, this fact is directly related to lack of information on healthy eating and physical inactivity.
It has been noted the growing interest of researchers in exploring non-pharmacological treatments for psychiatric patients, since we have seen significant improvements in the quality of life of these patients, when reduced dosage or deleted the indication of these drugs. Thus, it is necessary greater awareness of physicians indicate these multidisciplinary treatments to their patients, such as nutritional care, exercise, behavioral and occupational therapy (art and music).
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.