OVERVIEW
Sickle cell disease (SCD) is a chronic disease caused by mutation of the HBB gene, leading to the replacement of β-globin with abnormal hemoglobin S in hemoglobin subunits.1 Sickled blood cells have a short lifespan and complications include blocked blood vessels, acute chest disorder, infection, organ damage and stroke.2 Hydroxyurea therapy was approved by the Food and Drug Administration (FDA) in 1998 and decreases the number of pain crises in sickle cell patients.3,4 It increases the level of fetal hemoglobin (HbF) in sickle cell patients, lessening hemoglobin S polymerization.5 There have been numerous dermatological side effects noted, including skin atrophy, palmoplantar keratoderma, alopecia, and cutaneous and mucosal ulcers.6
We describe a case of a leg ulcer in a patient with sickle cell disease on hydroxyurea. Painful hydroxyurea induced leg ulcers have been reported in patients with myeloproliferative disorders.7 It is plausible that hydroxyurea is the one of the causes of leg ulcers in sickle cell patients.
CASE REPORT
We present a 28-year-old African American male inmate with a 22-year history of SCD and acute chest pain. He was admitted to the hospital with acute sickle cell pain crisis (Hgb: 7.3 g/dL, PLT: 422×103/µL, WBC: 10.8×103/µL, HMT: 19.9%, MCV: 96.1fL) and a painful chronic left ankle ulcer. The patient started hydroxyurea treatment about 8-years-ago.
The ulcer first appeared 5-years-ago on the patient’s left ankle, with subsequent recurrences. In the past, the patient’s ulcer was treated with wound care and dressing changes as well as mupirocin and collagenase.
Physical Examination
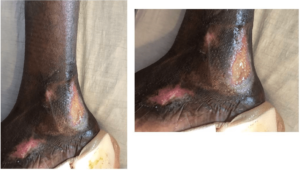
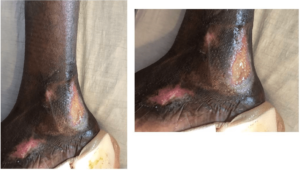
Physical examination showed stable vitals. Focused exam on the left ankle showed a unilateral ulcer (L: 2.5 cm, W: 1.5 cm, D: 0.2 cm) on the patient’s left malleolus. There were 2 smaller ulcers adjacent to the primary ulcer in various phases of healing. The primary ulcer was surrounded by post-inflammatory hyperpigmentation (Figure 1). There was no purulence or concern for infection with a pink healthy granulation tissue at the wound bed. Mild sero sanguineous discharge was noted.
Figure 1. Unilateral Ulcer
Vascular Examination
Venous duplex scan: There was no evidence of right or left lower extremity deep venous thrombosis. The right greater saphenous vein was patent and small. The left greater saphenous vein was also patent and small and was only identifiable in the thigh and knee area.
Noninvasive extremity arterial duplex: In the right lower extremity, the ankle-brachial index was 1.18, with multiphasic flow in the dorsalis pedis and posterior tibial levels. In the left lower extremity, the ankle-brachial index was 1.20, with likewise multiphasic flow in the dorsalis pedis and posterior tibial levels. It was concluded the patient had normal bilateral lower extremity arterial perfusion.
Magnetic resonance imaging lower extremity: Based on the magnetic resonance imaging (MRI), there was no evidence of osteomyelitis. Patchy heterogeneous fluid signal within the marrow was identified and likely a secondary to osteopenia. Mild plantar fasciitis was confirmed. Based on results, non-specific subcutaneous edema was likely reactive or secondary to third spacing.
Treatment
The recommended wound care for the ulcer included daily cleaning with wound cleanser, covering with foam dressing and securing with Tubigrip for compression and prevention of swelling. Medications prescribed for the wound care included cadexomer-iodine topical (Iodosorb 0.9% topical gel). Other medications prescribed to the patient included hydroxyurea, folic acid, ibuprofen, morphine and senna.
DISCUSSION AND CONCLUSION
Hydroxyurea is a widely used, safe drug with few long-term side effects. Common short-term side effects of hydroxyurea include decreased leukocyte, erythrocyte and platelet count.8 There are several other cases reporting painful hydroxyurea induced leg ulcers, mainly in patients with myeloproliferative disorders. These leg ulcers are generally close to the malleolus or on the lower limbs.9 The mechanism of hydroxyurea includes the inhibition of ribonucleotide reductase, leading to inhibition of S-phase and cell death.10 As a result, actively dividing basal keratinocytes forming the deepest layer of the epidermis may be damaged, leading to cutaneous problems and lower levels of collagen.6 Another potential cause of ulceration is megaloblastosis, a known side effect of hydroxyurea.11 Megaloblastosis can lead to enlarged RBCs, decreasing blood circulation in capillaries and depriving the basal cells of oxygen, which can hinder wound repair.12 Other causes of ulcers seen in sickle cell patient can be related to the underlying disease process itself including mechanical obstruction from sickling, thrombosis, bacterial infections and reduced nitric oxide availability.13
The mechanism causing hydroxyurea induced leg ulcers remains unclear, and the most recognized treatment option is cessation of hydroxyurea treatment. However, considering hydroxyurea usually decreases the rate of painful sickle cell episodes by 50% for sickle cell patients, more treatment options should be explored. From this case and other cases, it is suggested that wound care including wound dressings, bandaging and antibiotics cannot fully heal the ulcer and requires months of treatment.11,14 Potential alternative therapies include hyperbaric oxygen treatment which may increase the healing rate of the ulcer, topical application of Molgramostim and analgesics as well as the use of cultured skin grafts.13,15 Further studies are required to determine a better treatment option for sickle cell patients with hydroxyurea induced leg ulcers. It is also important for hematologists and internists to be aware of this complication of Hydroxyurea use. This prevents repeated work up for vascular causes of these ulcers.
CONSENT
The authors have received written informed consent from the patient.
ACKNOWLEDGEMENTS
None to declare.
FINANCIAL DISCLOSURE OR FUNDING
None to declare.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.