INTRODUCTION
The reliable and reproducible estimate of dry weight in hemodialysis patients remains a clinical problem to date. Prolonged overestimation of dry weight causes hypertension, left ventricular hypertrophy and heart failure, while the underestimation is responsible for a chronic dehydration leading to the risk of hypotension.1 Both complications have a significant impact on morbidity and mortality in hemodialysis patients.2
Despite the huge progress achieved in the assessment of the adequacy of dialysis treatment in term of solutes purification; no measure allows, at the present time, to accurately assess the adequacy of the fluid balance.3
Most centers determine the ultrafiltration rate during the session based on the weight «target» as a reference. This represents the weight reached late in the session after normalization of the patient’s extracellular volume. In other words, it is the weight that is associated with the absence of extracellular dehydration signs, or signs of hydrosodic retention.4 However, this parameter is considered clinically very subjective, varying significantly, and imprecise since it does not take into account the changes in nutritional status, lean body mass, and the vascular refilling capacity of each patient.5
It is obvious that using better assessment methods of determining volume changes during hemodialysis are needed to adapt the goal for fluid removal so that the target weight later will always be close to the true dry weight of the patient. Such methods have evolved from clinical assessment to sophisticated systems of “biofeedback”, which incorporate blood volume, ultrafiltration rate and conductivity, going through the use of Body Composition Analysis (Body Bioimpedance spectroscopy (BIS)), ultrasound of the vena cava, the serum markers and lung ultrasound.6
The objectives of our study are:
• To assess fluid status of chronic hemodialysis patients by using: lung ultrasound, Body bioimpedance spectroscopy (BIS), ultrasonography of the Inferior Vena Cava (IVC) and Natriurectic peptide type B dosage (BNP) assay,
• To measure the correlation between the results of the four methods,
• To compare the dry weight, determined by the objective methods mentioned above, with the one determined clinically,
• To identify associated factors with eventual errors in the clinical estimation of the dry weight.
MATERIALS AND METHODS
Study Design
This is a cross-sectional study, conducted during March 2014 in the hemodialysis center of Al Ghassani provincial Hospital in Fez.
Patients
Using an arteriovenous fistula, the patients included in
this study were aged over 18, and have begun chronic hemodialysis since at least 3 months.
Were excluded from the study all the patients with the following criteria:
• An acute event (infectious episode or a hospitalization) within the 3 months preceding the study regardless of the cause.
• A lung disease with pulmonary fibrosis, or dyspnea stage IV of NYHA showing a heart failure that may affect the results of lung ultrasound regardless of the state of hydration.
• Inability to wear bioimpedance spectroscopy (BIS) (prostheses, pacemaker …).
All our patients receive a conventional intermittent dialysis for two to three sessions per week, using low permeability polysulfone membranes with a standard bicarbonate dialysate. The Ultrafiltration rate is prescribed according to the interdialytic weight gains compared to the target weight clinically determined by the treating nephrologist.
Data Collection
The survey was carried out by a nephrologist not belonging to the team of hemodialysis center where the study is conducted. A pre-operating sheet was used for the collection of information.
In addition to demographic data and those related to kidney disease, comorbidities and dialysis prescription, we collected all episodes of intradialytic hypotension, cramps or postdialytic asthenia, during the last three sessions of hemodialysis.
The dry weight assessment parameters were measured in two phases: one hour before the Hemodialysis (HD) session and between 30 to 60 minutes following the end of the same session.
Therefore, the parameters collected are:
• Weight, under the usual conditions of the center using an electronic scale.
• The supine blood pressure measurement is done after 10 minutes rest, using a validated electronic device.
Bioimpedance spectroscopy (BIS):
We used the BCM (Body Composition Monitor, Fresenius Medical Care®, Germany), dedicated to the analysis of body composition and nutritional status of patients. The impedance was performed to the patients, who were lying down flat in bed, after having rested immediately 10 minutes before and 30 to 60 minutes after the hemodialysis session. The electrodes were placed on the wrist of the contralateral arm of the Arteriovenous Fistula (AVF) and on the homolateral ankle.
Lung Ultrasound:
Lung ultrasound was performed by the same trained nephrologist, who did not have access to patients’ clinical data and also to the impedance results. The imaging was made by using an ultrasound (KOLTRON Magic Maestro) with a 7 Mhz vascular probe in order to look for an alveolar-interstitial syndrome characterized by the presence of specific artefacts called “B-lines” or “comet tails “ which are proof of pneumonitis (congestion of the lungs) caused by fluid overload in hemodialysispatients.7,8 Ultrasound examination was performed to the patients in supine position, with a longitudinal scan from the second to the fourth intercostal space of the left hemi-thorax and from the second to the fifth intercostal space of the right hemithorax at the medioclavicular and midaxillary lines of each side. B-lines were defined as a hyperechogenic linear artifact that are emerging from the pleural line, going to the bottom of the screen, and are being coherent with respiratory movements. The number of B-lines has been determined by the sum of the B-lines found in each examined site. Thus, the selected number reflects the extravascular accumulation of the liquid in the lung.
Ultrasound of the inferior vena cava (IVC):
We used an ultrasound (KOLTRON Magic Maestro) with a 3.5 Mhz cardiac probe. The same trained operator explored the IVC within the sub-xiphoid window at 2.5 cm of the IVC-right atrial junction. The measure of the minimum diameter of IVC (DIVC min) was made during inspiration and during the expiration; the maximum diameter of the IVC (DIVC max) was measured.
Dosage of natriurectic peptide type B (BNP):
We assayed the BNP immediately before and after the hemodialysis session using a patented enzyme immunoassay (TOSOH®).
STUDIED VARIABLES
Definitions
• The subjective target weight: it was the prescribed weight taken from the patient logbook, estimated by the attending nephrologist, and based on clinical criteria such as: weight, blood pressure, presence of edema or vascular congestion, as well as the weight on cardiac index measured by the chest x-ray.
• The objective Target weight: it was the determined weight based on the various performed techniques (Impedance, BNP, lung ultrasound, ultrasound of the inferior vena cava).
• Weight loss: is the difference between the weight before and after hemodialysis.
Impedance Results
The reference values determined by the impedance to define euvolemia in the normal population are within the range of -1.1 L to 1.1 L.9 Referring to these values, we have classified our patients into three groups:
• Dehydrated patients if the fluid volume is less than the reference value-1.1 L
• Patients in euvolemia if the volume of fluid is within the reference range±1.1 L
• Patients in overload if the fluid volume is greater than the reference value+1.1 L.
Results of the Inferior Vena Cava Ultrasound
The index of the IVC diameter (iIVCD) was measured by dividing the IVCD maximal and IVCD minimal on body surface (Dubois formula) to obtain respectively the iIVCD max, and the iIVCD min.
The collapsibility index of the IVC (CiIVC) was calculated by using the following formula:
[(IVCDmax – IVCDmin)/IVCD max × 100].
Referring to the criteria of ultrasound,10 we classified patients:
– Dehydrated if the iIVCD max <8 mm/m².
– Euvolemic if 8 mm /m²≤iIVCD max ≤11.5 mm/m².
– In overload if the iIVCD max >11.5 mm/m².
Results of Lung Ultrasound
Pulmonary congestion (Lung congestion) by fluid overload was retained in patients with the following characteristics:11
1. Scan which shows several lines “B”: number >2 (criteria of the SFAR)
2. Positivity diffuse in more than one scans
3.Bilateral positivity
Biological Outcomes
For the BNP assay method used in our study, values that are below 120 pg/ml are considered as normal; whereas, those above 400 pg/ml are considered as high.12 For the other biological parameters, we used the mean value of serum sodium, calcium, phosphate, CRP, hemoglobin, PTH and albuminemia in the last three months.
STATISTICAL ANALYSIS
The data were entered into an Excel sheet and analyzed using SPSS software Version 20. In the descriptive analysis, quantitative variables were expressed as mean±standard deviation and qualitative variables as percentages. The comparison of means was made using Student test; whereas, the comparison of percentages was performed using Chi-square test. To measure the correlation between the results of the four evaluated objective methods, we have used the bivariate correlation method and estimated the r coefficient for each correlation. Subsequently, three groups of patients were defined according to the difference between the objective target weight determined by the different methods used in our study and the subjective target weight predetermined clinically by the health care team:
– Group A: The objective target weight is less than the subjective target weight with a deviation of more than one kilogram
– Group B: The deviation between the objective and the subjective target weight does not exceed one kilogram. This is the standard acceptable gap in our study.
– Group C: The objective target weight is greater than the subjective target weight with a deviation of more than one kilogram.
An univariate analysis was performed to show the correlates of the subjective estimation error of the target weight.
ETHICAL CONSIDERATIONS
An informed consent for participating in the study was obtained from all patients. No invasive investigation was used. All additional costs associated with the study were funded by the research budget of the Nephrology Department of the University Hospital Hassan II of Fez.
RESULTS
We included 77 patients, aged 48.13±16 years with a sex ratio (M/F) of 1.1. The average length of hemodialysis was 10.1±0.5 years. Initial nephropathy was vascular, glomerular and diabetic in respectively 35%, 20% and 8.5% of cases. 44% of patients are hypertensive. Dyspnea was found in 35.1% of cases, mostly stage I (24.7%) and no patient had dyspnea stage III or IV. Anemia was found in 52.6% with a mean hemoglobin rate of 9.62±2.17 g/dl. The mean albumin rate was 39.73±7.5 g/l. Clinical, biological and demographic characteristics are presented in Table 1.
Table 1: Baseline characteristics (mean±SD).
|
Parameters
|
N=77
|
|
Hypertension (%)
|
44
|
|
Cardiac ejection fraction (%)
|
66.5
|
|
Dyspnea stage (NYHA %)
Stage I
Stage II
Stage III. IV
|
35.1
24.7
10.4
0
|
|
Intradialytic hypotension (%)
|
7.8%
|
|
Weekly sessions (%)
3 times
2 times
|
50.6%
49.4%
|
|
Residual diuresis (ml/j)
|
146±394
|
|
Rate UF/session (ml)
|
2500 IQR (2000-3100) Range (1000-4500)
|
|
Hemoglobin rate (g/dl)
|
9.6 IQR (8.0-11) Range (4.8-14.1)
|
| Albumine rate (g/l) |
40.9 IQR ( 36-44.9) Range (20.3-48)
|
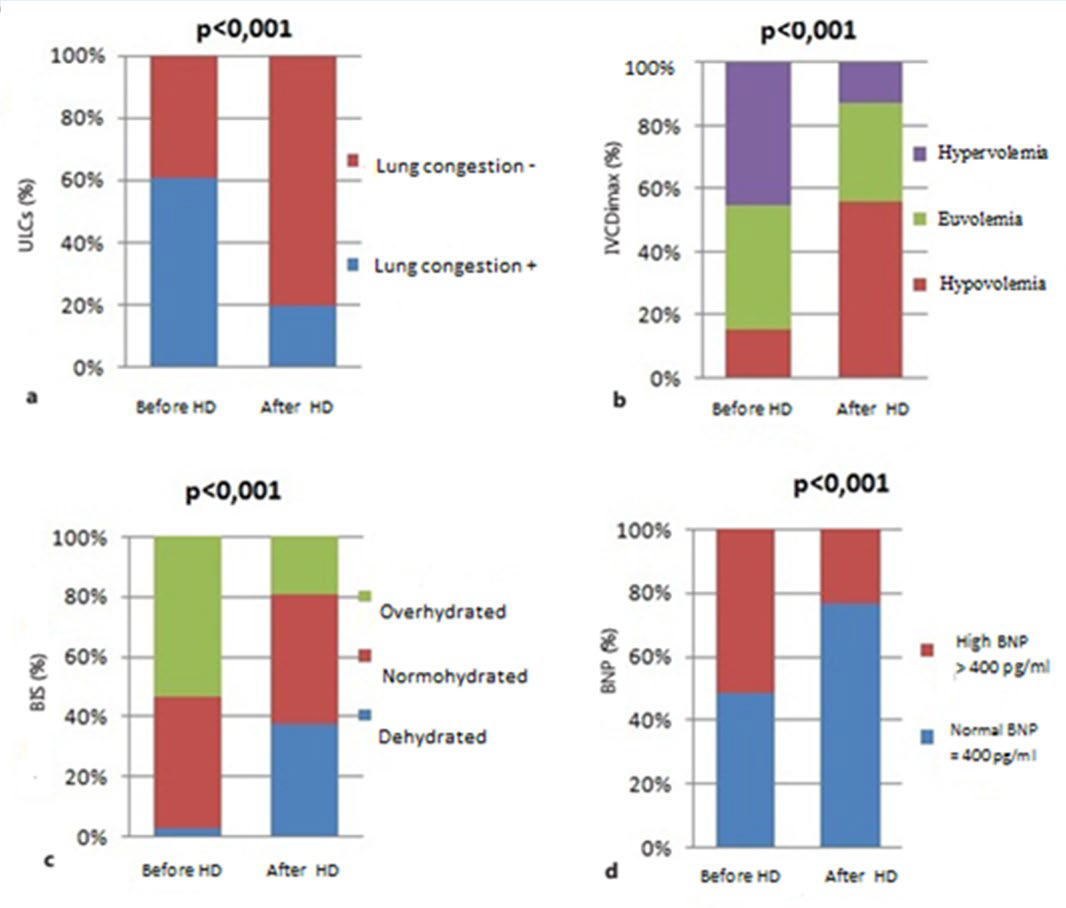
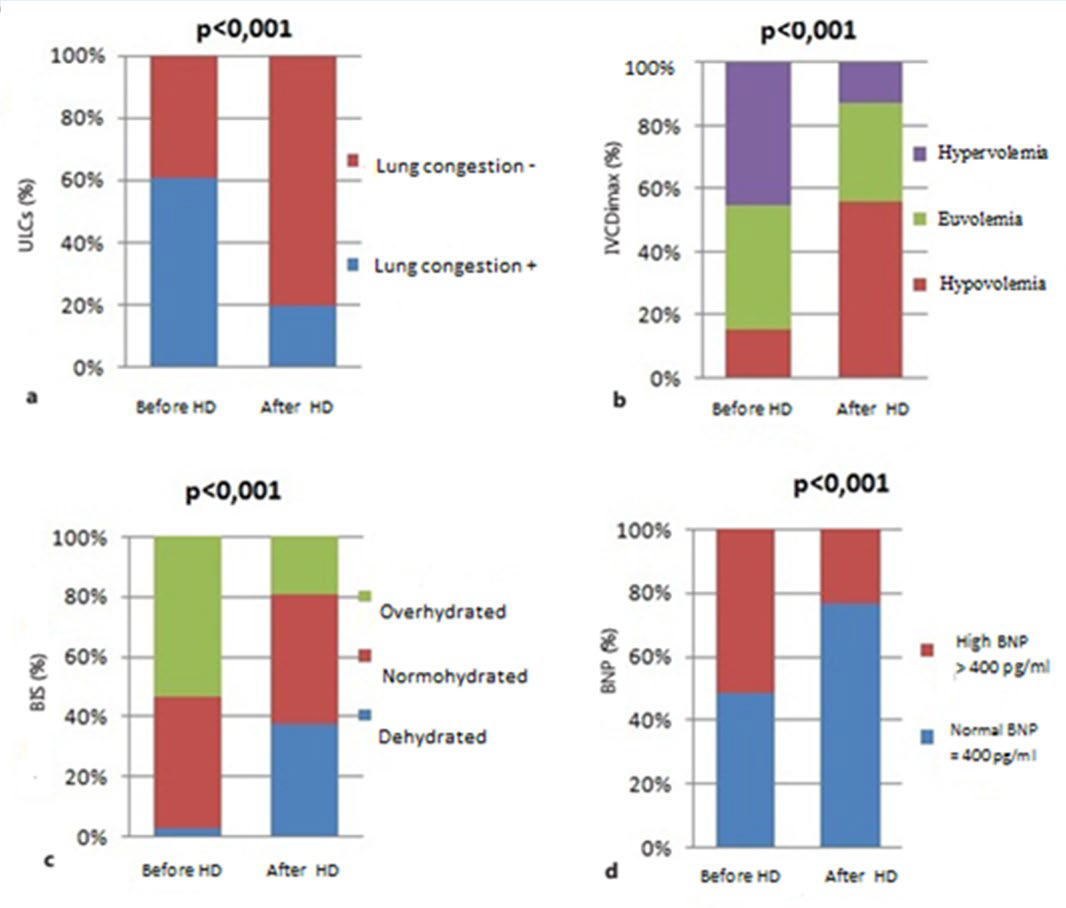
The values of fluid status assessment, which are measured by the impedance, the number of B-lines in lung ultrasound, the IVC index, and the BNP rate, decreased significantly (p<0.001) after hemodialysis compared to predialytic values (Table 2). The same results were shown when we consider the categories of each measurement method: in patients with fluid overload, the values of impedance, IVC, the number of B-lines and BNP decreased significantly subsequent to hemodialysis (Figure 1). On the other hand, in post dialysis, there were more patients who were classified hypovolemic by ultrasound of the IVC (57%) than by impedance (38%).
Table 2: Fluid status before and after hemodialysis session (mean±SD).
|
Before HD
|
After HD |
P
|
|
Bioimpedance (liter)
|
+1.2±1.2
|
-0.36±1.3 |
<0.001
|
|
Lung ultrasound Number of B-lines
|
4.4±3.4
|
1.3±1.6 |
<0.001
|
|
Ultrasound of VCI iDVCI max (mm) iDVCI min (mm)
CVCIi %
|
10.2±2.6
5.1±3.1
53.2±24.1
|
7.6±2.6
2.4±3
75.1±29.2 |
<0.001
<0.001
<0.001
|
|
BNP (pg/ml)
|
603±606.5
|
405.5±560.7 |
<0.001
|
VCI: Inferior vena cava; iDVCI: index of the inferior vena cava diameter; CVCI: Collapsibility index of the inferior vena cava; BNP: B natrialpeptid
Figure 1: Distribution of groups according to fluid status determined by lung ultrasound comets (a) inferior vena cava diameter (b) bioimpedance spectroscopy (c) and b natrial peptid (d) before and after hemodialysis session.
The correlation analysis between the results of different techniques before and after hemodialysis is summarized in Table 3. There was a very significant correlation between the impedance, lung ultrasound, the index of the maximum and minimum IVC and its collapsibility both before and after hemodialysis session. However, there was not any significant correlation between BNP rate and other studied methods.
Table 3: Correlation between different techniques before and after hemodialysis session.
|
B-Lines
|
iDVCI min |
iDVCI max |
CVCIi |
BNP
|
| – Before hemodialysis session |
|
|
|
|
|
|
Over hydratation by bioimpedance
|
0.691**
|
0.372** |
0.461** |
-0.244* |
0.08
|
|
B-Lines
|
_
|
0.610** |
0.607** |
-0.485** |
0.095
|
|
iDVCI min
|
_
|
_ |
0.788** |
-0.558** |
0.052
|
|
iDVCI max
|
_
|
_ |
_ |
-0.916** |
0.013
|
|
CVCIi
|
_
|
_ |
_ |
_ |
-0.005
|
|
BNP
|
_
|
_ |
_ |
_ |
_
|
| – Afterhemodialysis session |
|
|
|
|
|
|
Over hydratation by bioimpedance
|
0.756**
|
0.559** |
0.581** |
-0.507** |
0.128
|
|
B-Lines
|
_
|
0.679** |
0.749** |
-0.592** |
0.101
|
|
iDVCI min
|
_
|
_ |
0.837** |
-0.959** |
0.001
|
|
iDVCI max
|
_
|
_ |
_ |
-0.737** |
0.097
|
|
CVCIi
|
_
|
_ |
_ |
_ |
0
|
|
BNP
|
_
|
_ |
_ |
_ |
_
|
|
*0.001<p<0.05 **p<0.001
|
|
|
|
|
|
VCI: Inferior vena cava; iDVCI: index of the inferior vena cava diameter; CVCI: Collapsibility index of the inferior vena cava; BNP: B natrial peptid.
We also studied the correlation between the change of the ultrasound results and the movement of water during hemodialysis session expressed by weight loss. Only the reduction of the number of the B-lines was significantly correlated with weight loss (β coefficient=0.36, p<0.005) (Table 4).
Table 4: Linear regression with weight loss
|
Correlation between weight loss and:
|
Coefficient β |
P
|
| B-linesreduction (%) |
0.36
|
0.005
|
|
DVCI max reduction (%)
|
0.12 |
NS
|
| DVCI min reduction (%) |
0.04
|
NS
|
| CVCI reduction (%) |
-0.11
|
NS |
DVCI: the inferior vena cava diameter; CVCI: collapsibility of the inferior vena cava.
In our study, only 15.6% of patients did not have a gap between the subjective target weight and objective target weight, while 84.4% of patients had a significant difference between the results provided by the techniques studied and the result of clinical evaluation. 70.1% of these patients had a negative gap (group A) and 14.3% of them had a positive gap (group C).
In the univariate analysis, several factors were studied in order to show correlates of these differences including: age, sex, comorbidities, length of hemodialysis, inflammation, anemia, nutritional status, left ventricular hypertrophy, systolic ejection fraction. Age was the only significant factor that was related to the differences since the patients with a negative gap (group A) had an average age of 47.2±12 years; whereas, the subjects with no gap (Group B) had an average age of 58±13 years and those with a positive gap (group C) had a mean age of 50.7±13.7 years (p<0.04).
DISCUSSION
This is a cross-sectional study conducted to compare firstly the different techniques of assessing water status before and after hemodialysis session, and secondly to assess hydration status of our patients and have a more objective view of their dry weight in order to establish a strategy to optimize their care.
This is a cross-sectional study conducted to compare firstly the different techniques of assessing water status before and after hemodialysis session, and secondly to assess hydration status of our patients and have a more objective view of their dry weight in order to establish a strategy to optimize their care.
All the techniques investigated in this study show that there is a reduction in overload after hemodialysis session, and there is a good correlation between these different methods except the BNP assay. This result fits in with the one found by F Basso, et al. in 2013.13 Although, the new techniques are promising, they have important practical and theoretical limits. For example, skin lesions, wrongly placed electrode, electrical interference, and obesity are the limits of theimpedance.6 In addition, the data of the impedance change 120 minutes after the end of hemodialysis.14 Similarly, Agarwal, et al. has shown that the measurement of IVCD is a method that well reflects the intravascular volume but has a low sensitivity for detecting a change in the fluid in post-dialysis time.15 Consistently, our results shown that inpost-dialysis, there are more patients classified hypovolemic by ultrasound measurements of the IVC than by conductivity measurement. This difference is due to the time required for transferring the fluid from the interstitial sector to the intravascular one “refilling’’. At the end of the hemodialysis session, a relative hypovolemia may exist. The conductivity measurements achieved just after the dialysis session, underestimate the degree of dehydration. While ultrasound of inferior vena cava (IVC) overestimates the degree of dehydration in these patients. The results obtained by these two techniques should be close enough if the measurements were made a few hours after hemodialysis session.16 Among our hemodialysis patients, the rate of BNP is high in pre-dialysis, especially in patients suffering from over load, and significantly reduces in post-dialysis time. However, it is not correlated with the results of the other methods. This could partly be explained by the existence of other determinants than the volume overload that may influence BNP rate in these patients, particularly any myocardial aggression.17 On the other hand, this hormone is dialyzable with the membranes of high and low permeability.18 This allows us to infer, as it has already been shown, that the dosage of the BNP does not have an interest in the evaluation of water status in hemodialysis patients,19 since this assay does not distinguish between euvolemic and dehydrated patients.20
Lung ultrasound is a simple method, that is easy, inexpensive, without irradiation, andwhich can be used at the bedside of the patients.21 Nevertheless, it is an operator-dependent method. Previously, it was shown that the number of B-lines was correlated to the extravascular water.21 In our study, the correlation between weight loss and ultrasound data, showed that only the reduction of B-lines was significantly correlated; whereas, no correlation existed with the reduction of IVCD. This confirms that the two preceding techniques evaluate two different fluid compartments: the IVCD reflects the volume of intra-vascular water, and the number of B-lines reflects the volume of extravascular water. Thus, the IVCD is not sensitive in assessing rapid changes of fluids during hemodialysis,22 whereas, lung ultrasound can be performed immediately after hemodialysis.23
At the end of this study, we had shown that a significant difference existed between the objective target weight and the subjective target weight. This confirms that the actual determination of the dry weight is difficult and the clinical estimation remains a non-specific method3 and therefore insufficient. The underestimated dry weight in most of our young chronic hemodialysispatients had no clinical or interdialytic relevance. It misled the nephrologist in 70% of cases. This would be due to a better hemodynamic tolerance of Ultrafiltration or rather of dehydration in young patients who have a good cardiovascular condition. Studies have clearly shown an increased risk of death and cardiovascular events when intradialytic hypotension happens in hemodialysis patients in older population.24Young hemodialysis patients, asymptomatic despite the hypovolemia, are often underestimated in different studies. Cardiovascular morbidity and mortality risk deserves to be studied in this subgroup of patients. It also raises the question of the value of a periodic systematic use of impedance and ultrasound techniques in all hemodialysis patients even in the absence of a clinical anomaly.
CONCLUSION
This study is among the few studies that have used lung ultrasound to assess the state of hydration of hemodialysis patients. It allows us to show the right correlation between the results of this review and those of the impedance and the ultrasound of the IVC. The existence of a gap between the subjective target weight and the objective target weight suggests the incessant need for a coupling between these different techniques according to a strategy adapted to the characteristics of each patient.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
ACKNOWLEDGEMENT
The abstract of this study has been selected by the scientific Program Committee for moderated poster presentation at the World Congress of Nephrology 2015.