COMMENTARY
Cardiovascular disease has a huge impact on our society and the individuals affected. According to the most recent data published by American Heart Association (2014 Update), Coronary heart disease alone caused about 1 in 6 deaths in the United States in 2010. Each year about 620,000 Americans have a new coronary attack and about 295,000 have a recurrent attack. The total direct and indirect cost of CVD and stroke in the United States for 2010 is estimated to be $315.4 billion.1 As the national focus continues to be on health care utilization, care and quality it becomes increasingly important that we try to address the multiple modifiable risk factors that have been shown to improve cardiovascular outcomes. Very little has been published regarding comprehensive prevention in a combined approach utilizing a cardiovascular prevention clinic.
In 2010, the senior author attempted to explore the concept of truly comprehensive cardiovascular preventive clinics with goal driven protocols and operated by mid-level providers with different backgrounds from clinical pharmacy to advanced nurse practitioners. The vision of the clinic was to streamline cardiovascular screening, medical management, and prevention programs in order to provide more efficient and higher quality care for the service members with ultimate goal
of reducing long term outcomes and cost utilization. The clinic currently utilizes a clinical pharmacist, physician assistant, and advanced nurse practitioners as well as an exercise physiologist and technicians with peripheral support by nutrition and psychology and supervised by the founder and the senior author, Ahmad M. Slim. Currently, the clinic evaluates for and treats lipid disorders, Hypertension (HTN), Diabetes Mellitus (DM), Peripheral Arterial Disease (PAD), Screening Abnormal Calcium Score, Tobacco dependence, and provides weight loss management and dedicated exercise program for weight loss and claudication treatment. Screening and treatment is based on the most recent evidenced-based guidelines published and updated annually,2,3,4,5 and written up into strict standard operating procedures for all mid-providers within the clinic to follow. The clinic is part of the patient centered home model with a multi-disciplinary approach.
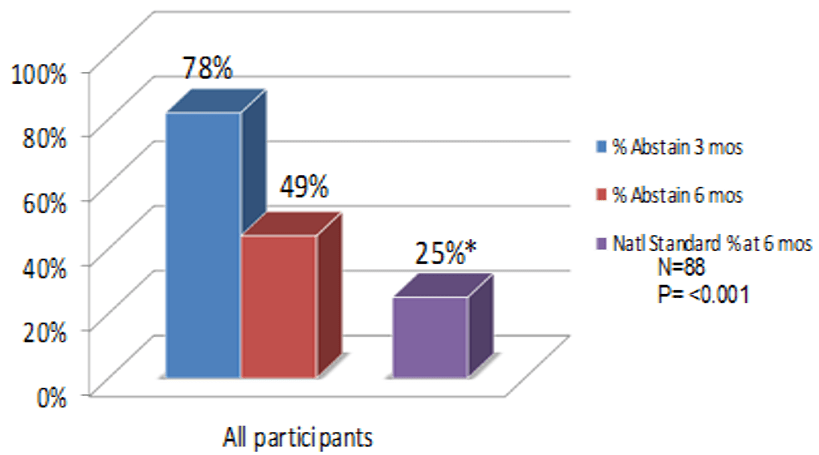
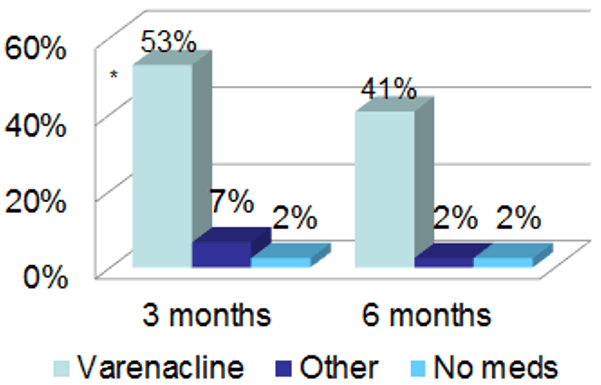
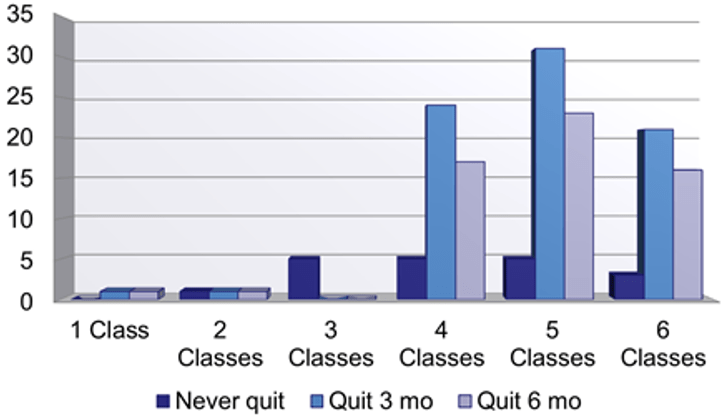
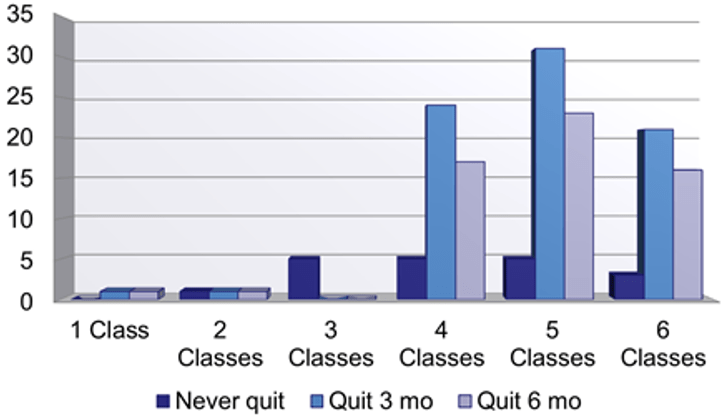
The current patient demographics based on preliminary review for quality assurance and process improvement purpose produced 1800 patients with 60% male predominance and an average age of 64 years+/- 10.4. The average Framingham Risk Score was 14%+/- 8.3%, diabetics compromised 30%and smokers 15% of the population. 221 patients had an abnormal calcium score upon enrollment with an average score of 178 ± 323. Data on 88 participants enrolled in the smoking cessation program collected includes class attendance, cessation, and abstinence rates at 1, 6, and 12 months. Initial pull showed that participants in the smoking cessation classes were very successful with 78% abstinence at 3 months and 49% abstinence at 6 months compared to 25% for the national average (Figure 1). We evaluated the impact of class attendance as well as type of intervention utilized on regular basis to constantly improve delivery of care and implement changes that will maintain the success rate or improve it (Figure 2 and 3). The data shows a significant improvement in smoking cessation rates when patients use Varenicline (Chantix®) as compared with other medication or no medications and also when patients attend 4 or more cessation classes.
Figure 1: Abstinence rates vs. the National average. *Hunt WA, et al. J Clinical Psych, 1971; 27:455-56
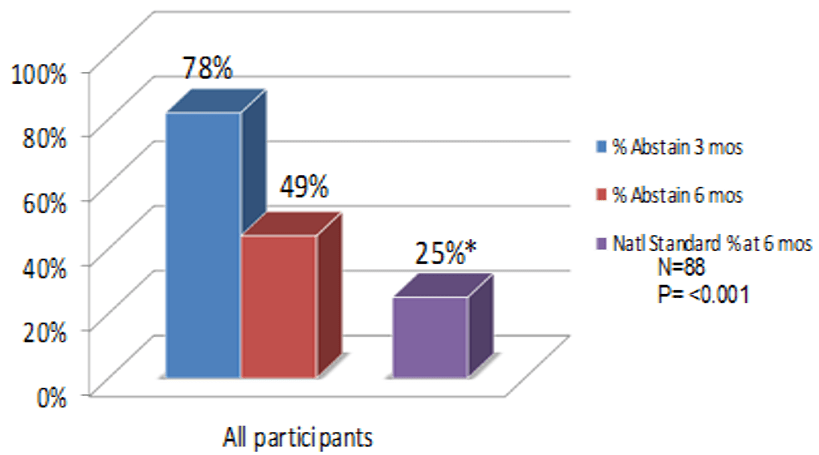
Figure 2: Abstinence Rates by Medication (Completed Course)
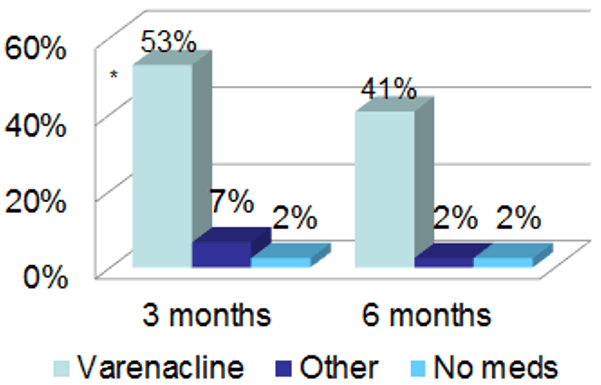
Figure 3: Class attendance and Cessation
The preventive cardiology clinic goal for lipid management was for LDL cholesterol to be less than 100. Data pulled on 1800 patients showed that 38% of patients were at goal prior to being seen by the clinic and a significant increase to 78% of patients with LDL cholesterol at goal was seen. Figure 4 shows these stats as compared to current HEDIS measures with a goal of 40%. These percentages are also significantly better when compared to only 18% of patients with CHD meet a goal LDL<100.6
Figure 4: Pre vs. Post Preventive Cardiology Clinic LDL goal comparisons

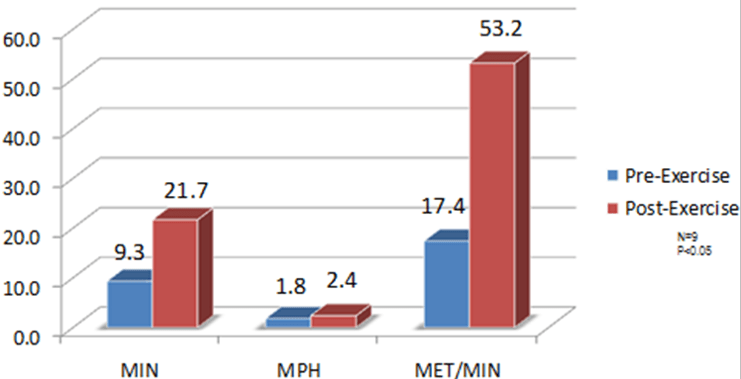
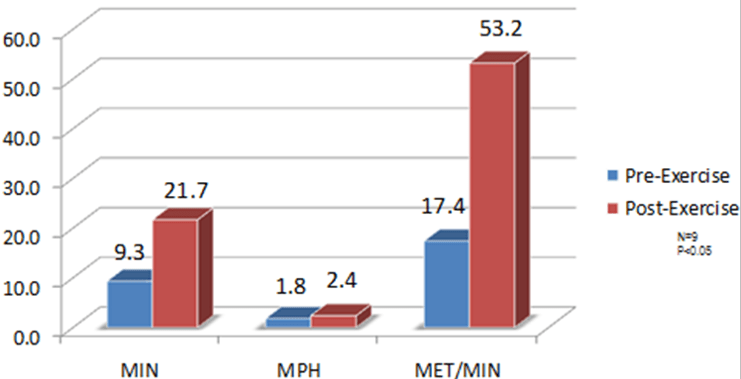
The initial vascular data is also promising, 9 patients were found to have vascular disease and participated in a structure exercise program in order to try to help increase their exercise capacity. The patients underwent supervised exercise therapy in a cardiac rehab facility. The patients had 5 sessions per week (2 were supervised) where they exercised on a treadmill to near maximal claudication pain. The participants were in the program for greater than 3 months and the results showed significant improvements in walking distance and overall quality of life. The patients were able to increase the amount they could exercise on average from 9.3 minutes to 21.7 minutes and also increase their speed from 1.8 mph to 2.4 mph after completing the exercise program (Figure 5). In addition to the above data regarding tobacco cessation, lipids, and exercise improvement, there are additional endpoints that were successful with regard to blood pressure management, coronary calcium score, and diabetes management. The additional data will follow in a more comprehensive data pull in a future article.
Figure 5: Improvements in exercise capacity in peripheral artery disease patients
In summary, the concept, design and implementation of the Preventive Cardiology Clinic at Brooke Army Medical Center using a multi-disciplinary approach with evidence based protocols and standard operating procedures in a patient-centered design enhanced patient participation and optimized success in preventive care in a high-risk population. This work aligns with published data from 10 European countries and Israel where primary care systems with cardiovascular disease focus had better overall outcomes and strength as compared to programs with broad overall life style modification program.7
The Preventive Cardiology Clinic resulted in improved identification and screening of cardiovascular patients at risk, improved implementation of preventive therapies and achievement of target goals, significantly affected tobacco cessation success rates that surpasses nationally reported success rates, and improved quality of life. We feel this concept could be easily replicated using existing resources in most military and other medical treatment facilities.
CONFLICT OF INTERESTS
The opinions in this manuscript do not constitute endorsement by San Antonio Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, Department of Defense, or the U.S. Government of the information contained therein. The authors declare that there is no conflict of interests regarding the publication of this article.