INTRODUCTION
The determination of lung volume are technically challenging and involves rather elaborate techniques that vary from: (i) helium dilution, where a closed-circuit spirometer apparatus is filled with a mixture of gas in the lung with a known volume of gas containing helium and oxygen; (ii) nitrogen (N2) washout, where the technique is based on the participant inhales 100% O2 and exhales through a one-way value measuring N2 content and volume; (iii) body plethysmography, where changes in lung volumes that accompany compression or decompression of the gas in the lungs during respiratory manoeuvres, and (iv) using imaging techniques such as conventional radiographs, computerised tomography, magnetic resonance imaging, where images at the time of lung inflation can provide estimates of lung volumes.1,2,3
Lung volumes derived from conventional direct measures are usually based on the volumes within the outlines of the thoracic cage and the volume of tissues, as well as the lung gas volume.3,4 Indirect methods following maximal exhalation using spirometry have been commonly used as an less technically challenging estimation of residual lung volume.1,4-8 Typical measures with spirometry include: (i) vital capacity (VC) and its two subdivisions (a) slow vital capacity (SVC) which is the maximal amount of air exhaled steadily from full inspiration to maximal expiration and is not time dependent and (b) forced vital capacity, which involves the volume of lungs from full inspiration to forced maximal expiration. (ii) forced expiratory volume in one second (FEV1) where the volume of air is expelled in the first second of a forced expiration (iii) forced expiratory ratio (FER %) is the percentage of FVC expelled in the first second of a forced expiration ((FEV1/FVC) x100) (iv) forced expiratory flow between 25-75% (FEF 25-75%) (also known as the maximum mid-expiratory flow (MMEF)) this is the expiratory flow rate in the middle part of a forced expiration.
There is an assumed value of 0.9-1.6 L in a normal healthy adult male6,8; however, any assumptions in the determination of residual lung volume may lead to errors in body volume as large as ±0.5 L for a given individual, thus leading to an underestimation of Db.10 A study by Wanger et al2 compared various direct and indirect methods and results indicated that body plethysmography yielded higher results than helium dilution, nitrogen (N2) washout and spirometry. Therefore, with such extensive measures, evidence suggests that it is still difficult to reach a consensus where all lung volume measures are in agreement.1,7 Therefore, the aim of this investigation was to investigate the agreement of the estimation of residual lung volume from three possible approaches. These included, a ‘spirometry’ method (via spirometry),1,3,9 application of regression equations following ‘panting’ method (via the air displacement plethysmograph (BOD POD®))4,6,8,9 and a general ‘prediction’ method (based on age, gender, ethnicity and stature10,11,12,13 to estimate Db.
METHODS
Twenty two participants (n=10 male and n=12 female) were recruited from the University of Gloucestershire, undergraduate programmes. All participants were over 18 years of age and all were free from disease, illness or injury (͞χ±s; age=20.5±1.7 years, body mass=68.7±1.5 kg and stretched stature=172.0±8.3 cm). Participants completed a Health Questionnaire and this information was used in processing a flow diagram to determine whether the participants were eligible to take part in the testing. If eligible, the participants were requested to give written informed consent and they understood their rights to withdraw. In order to carry out three approaches to estimate residual lung volume, the following data processes were undertaken by all participants.
The ‘Spirometry’ Method
All participants sat in an upright position and applied a nose clip, whilst holding the Spirometer (Micro Medical Micro Loop Spirometer model 3535) breathing tube in their dominant hand. A rate of breathing for the participant was called by the rater which comprised of three cycles of inhalation and exhalation. On the third cycle call, the rater asked the participant to take a large inhalation and then a maximal exhalation that was blown out through the tube. Each participant was given three attempts to obtain their best forced vital capacity (FVC) value. The greatest FVC value was corrected for body temperature and pressure saturated (BTPS) that was determined by using a correction table.14 Finally the corrected FVC value was transferred to the spirometry equation dependent upon gender of each participant:
LVspir = FEV (BTPS) (L) x 0.24 – (males)
LVspir = FEV (BTPS) (L) x 0.28 – (females)
LV=lung volume; FVC=Forced vital capacity; BTPS=body temperature and pressure saturated14
The ‘Panting’ Method
All participants followed a measurement protocol, with step by step instructions given on the BOD POD® system computer. Participants were asked to apply the nose clip and hat and enter the BOD POD® and sit with an erect posture with their hands folded on their laps and feet placed on the floor of the chamber. The chamber door was then closed and sealed. During the test, participants were instructed to put the breathing tube (that was connected to the BOD POD®) in mouth and follow the cadence displayed on the screen by breathing in and out of the tube. Between the 4th and 6th breath a message alert appeared on the screen ‘prepare to puff’. During exhalation the breathing tube closed for 2 s and coincided with the message ‘puff, puff, puff’ on the screen. Participants were required to puff gently three times whilst maintaining a tight seal between the mouth and tube. At the end of the 3rd puff the measurement was completed (after ≈ 3-5 minutes) derivation of lung volume (l) was provided via the BOD POD® system computer, using the following equation:
LVpant = TV/2 (L) + FRC (L)
Where: LV=lung volume; TV=tidal volume; FRC=functional residual capacity (Life Measurement Inc.,)15
The ‘Prediction’ Method
In order to calculate the predicted residual lung volume participants age (y) and stretched statue (cm) were required. Once obtained, the data was then transferred to the equation derived by Crapo et al1 and a single value recorded:
LVpred (L)=0.410x(stature (cm))-(0.210 x age (years))-26.31
Where: LV=lung volume (Crapo et al11)
Data analysis involved the construction of scatter plots to determine the linear relationship between the three estimation methods of spirometry, panting and prediction from all participants and by applying the 95% limits of agreement (LoA) method to quantify the bias, random variation and heteroscedasticity. These analyses provided illustrative examples to see the deviation from the line of identity and to determine whether significant differences (under-reporting) were evident between the three estimation methods.
RESULTS
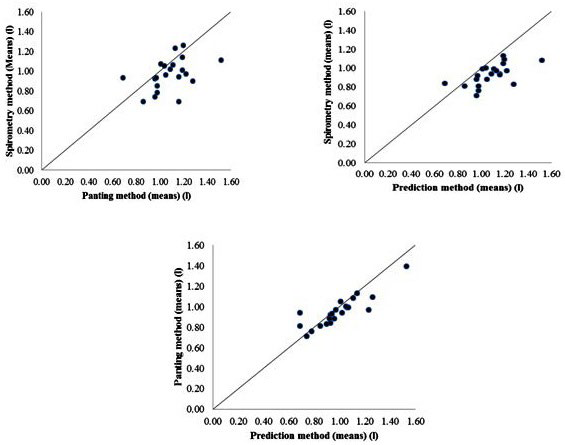
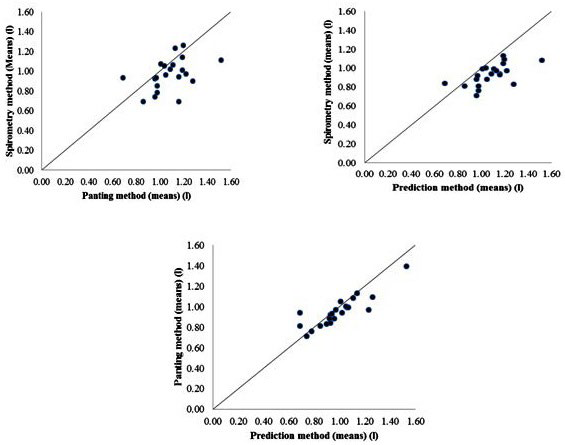
Three scatter plots are provided for illustrative purposes to demonstrate the linear relationship between the separate measures of residual lung volumes as shown in Figure 1. Linear relationships between the three residual lung volume measures were found, but closer inspection of Figure 1 did show some deviation from the line of identity, particularly with the spirometry – panting and spirometry–prediction method. Although, it is important to note this linear relationship was expected given that they are measuring the same variable.
Figure 1. Comparison between Spirometry and Panting Methods; Spirometry and Prediction Methods and Panting and Prediction Methods for Estimating: Lung Volumes (l).
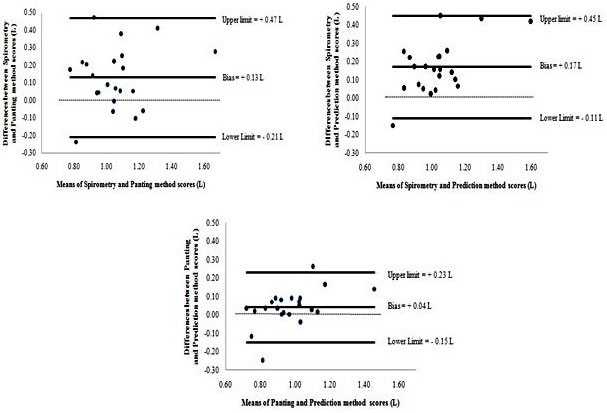
Due to the expected linear relationships found in Figure 1, further analytical investigations were needed to determine the agreement between the three different approaches to estimate residual lung volume. Bias, random variation and 95% limits of agreement approaches were then applied, and illustrated in Figure 2.
Figure 2. Bland and Altman Plot Showing Bias and 95% Limits of Agreement for the Spirometry and Panting Methods (Note: Direction of Bias [Panting–Spirometry]); Spirometry and Prediction Methods (note: Direction of Bias [Prediction–Spirometry]) and Panting and Prediction Methods (note: Direction of Bias [Prediction–Panting]) for Lung Volumes (l).
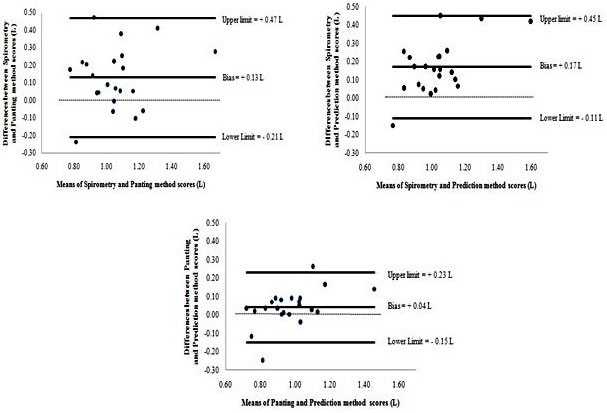
Evidence from Figure 2 indicated there was a bias of 0.13, 0.17 and 0.04 l for the panting, spirometry and prediction estimation techniques and limits of agreement of 0.47 to -0.21, 0.45 to -0.11 and 0.23 to -0.15 L respectively. To quantify these findings, if for example, a new participant (not one from the n=22 sample) measured 1.2 L for residual lung volume there is a 95% probability that when measured using the spirometry, panting, and prediction estimation techniques, estimation of residual lung volume can be estimated as low as 1.2 L-0.47=0.73 L to as high as 1.2 L+0.21=1.4l L; 1.2 L-0.45=0.75 L to as high as 1.2 L+0.11=1.31 L and 1.2 L-0.23=0.97 L to as high as 1.2 L+0.15=1.35 L respectively. Over all these findings suggest that the spirometry technique demonstrated a more accurate estimation of residual lung volume by 0.29 L when compared to panting and prediction estimation techniques. Whilst it is important to recognise that these differences, albeit small, they could potentially overestimate residual lung volumes and consequently underestimate Db.
CONCLUSION
Results from this investigation showed linear relationships between the spirometry and panting methods and the spirometry and prediction methods for estimating residual lung volumes; however, a stronger relationship between the panting and the prediction methods (Figure 2). It is important to note that these linear relationships were expected given they were measuring the same variable. In relation to limits of agreement data analyses, the bias was modest (0.17 L at worst), with the spirometry method giving lower values than both the predicted and the panting methods respectively. The best agreement (negligible bias and lowest limits of agreement) was between the panting and the prediction methods (0.04±0.19 L), although these methods provided higher values of residual lung volume. These findings suggest that the spirometry technique demonstrated a more accurate estimation of residual lung volume when compared to panting and prediction techniques.
Practical implications were also considered to reinforce the argument for the best measure to estimate residual lung volume. For instance, the panting method requires the use of the BODPOD®, whilst undertaking an unusual and sometimes problematic breathing technique and the prediction method is reliant on regression equations without practically measuring any lung volumes. Whereas the spirometry method uses standard (and the simplest) techniques to determine lung volumes and is considered the most widely used method within research determining Db from hydrostatic weighing.1,6,8,16 Research has suggested that studies that used alternative methods to spirometry such as panting and prediction methods should be treated with caution, as they are likely to overestimate residual lung volumes and consequently underestimate Db. 1,16 Thereby within body composition analyses, it is important to recognise the impact this underestimation could have on a participants Db if residual lung volume is not reliably measured. It was therefore concluded that given the absence of a criteria measure, the spirometry method would be the obvious measurement approach of choice for determination of residual lung volume for future research.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.