INTRODUCTION
Priapism is a persistent, usually painful, erection that lasts for more than four hours, occurs without sexual stimulation and is unrelieved by ejaculation. It was first described in 1845 by Tripe,1 as it is a relatively uncommon occurrence and as a result, there is scant contemporary literature on standardized treatment of males who experienced priapism. Two types of priapism, namely the ischemic priapism (also known as low-flow priapism) and non-ischemic priapism (or high flow priapism) have been well described. They both have specific and different causes1 and their management also vary from each other. The causative mechanisms even though not clearly understood, involve complex neurovascular factors. It may be associated with the use of intracavernous injections for erectile dysfunction, sickle cell disease (SCD), recreational drugs (cocaine and marijuana abuse), antipsychotic therapy, blood cancers like leukemia and perineal trauma.2,3 Adeyoju et al6 reported a high incidence (35%) of priapism among patients with sickle cell anemia which they identified as a common aetiological factor.
Badmus5 in an earlier study, also noted SCD as the commonest cause of priapism in southwestern Nigeria, whereas Aghaji2 in his series reported local aphrodisiac as the commonest predisposing factor of priapism in Eastern Nigeria followed by SCD. Whereas, use of intracavernous therapy is a common aetiological factor in the advanced countries, it is certainly rare in the poor resource settings like ours due to cost constraint and scarcity.2 Although, not all patients require immediate elaborate treatment, it is imperative to differentiate those requiring urgent intervention and offer such accordingly.7 Surgical shunts try to correct the priapic state by literally diverting blood from the rigid corpora cavernosa into the corpus spongiosum. Late presentation to the urologist is common and could be the result of ignorance both on the part of the patient with priapism and some healthcare providers. We carried out this review to determine the aetiology, pattern of presentation and outcome of surgical interventions for priapism in our setting. It is our hope that this will help to address some of the challenges occasioned by the management of this condition in developing countries like ours, remind us of the various surgical options and outcomes of treatment, and to increase public awareness to avert late presentation and hence mitigate the sequalae of erectile dysfunction associated with priapism.
PATIENTS AND METHODS
A retrospective analysis of data was extracted from patient’s case notes and operation register of the University Of Abuja Teaching Hospital from 2008 to 2013. Demographic information on age, duration of symptoms and predisposing factors were documented. Following full clinical examination the patient’s blood and urine samples were taken for full blood count, genotype and urinalysis. Broad spectrum antibiotics were routinely commenced and patients were prepared for surgery. Three common types of distal shunt procedures via winters, Ebbehoj and Al-Ghorab were carried out based on the surgeon’s discretion.
We improvised with a size 16 guage intravenous cannular in creating a winter’s shunt through the glans and then the corporal cavernosa. Ebbehoj shunt was performed with the use of a size 11 blade pierced longitudinal through the dorsal glans skin along the direction of the two corpus rods and turned 90 degree to create the shunt. The outcome of erectile function, where applicable was qualified as able to achieve penetrative intercourse (normal), erections not able to penetrate (partial) and no erections (complete). No standardized method of assessment of erectile function was used.
RESULTS
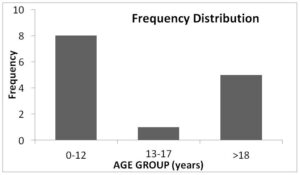
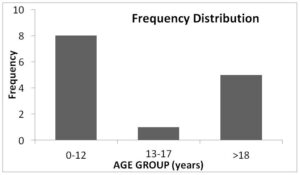
A total number of 17 patients (n=17) who had distal shunt procedures over the 5-year period were reviewed. The age range was 4-37 years with a median of 17 years (IQR 22.3). However, the median age among patients who had priapism attributable to sickle cell disease was 11 years (IQR 12.9) and a bimodal age distribution pattern (children 0-12 years and adolescents >18years) was obvious among the sickle cell disease patients (Figure 3).
DISCUSSION
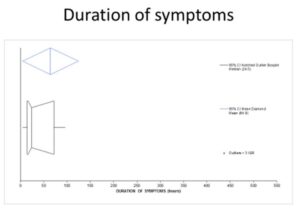
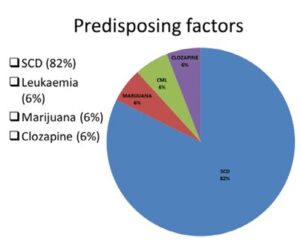
This review is amongst few reported series of priapism in our environment highlighting important issues regarding the mode of presentation and surgical management. We have assessed the outcome of procedures carried out in the treatment of priapism in our setting. Delay in presentation is common in our series as the median duration of symptoms prior to presentation is 24 hours. We have deduced that in our setting most patients are likely to present after 17-72 hours after the commencement of symptoms (Figure 1). Prior authors in this region have also reported late presentation of cases.2,3,5 This current study corroborates previous studies that sickle cell disease (Figure 2) is the most prevalent comorbidity (82%) associated with ischemic priapism.3,5 We have found a bimodal age distribution (Figure 1) among these subset of patients with peaks in the age ranges below 12 and above 18 years of age. The patient who had priapism following an overdose of cloxapine is on treatment for schizophrenia by the behavioral physician. Substance abuse with marijuana and leukemia are well-documented pre-disposing factors to ischemic priapism. 2,3,8,9
Figure 1: Boxplot Showing Median Duration of Symptoms Presentation to Intervention (24 hours) and the 95.1% Confidence Interval (17 to 72 hours). This Suggests that the Optimal Duration of Symptoms Prior to Presentation in our Environment (17 to 72 hours) is way beyond the Time before Onset of Damage Commences to the Corporal Tissues.
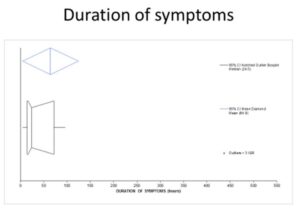
Figure 2: Pie Chart Depicting the Predisposing Factors to Ischemic Priapism. Sickle Cell Disease Accounts for the Vast Majority of Priapism (85%) in our Series. Other Pre-disposing Conditions are not as Common.
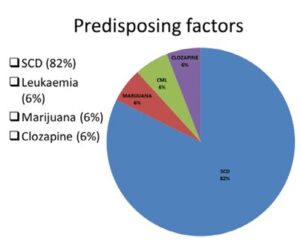
Figure 3: Bar Chart Showing the Bimodal Age Distribution of Priapism Among Sickle Cell Disease Patients. Most Cases of Priapism in Sickle Cell Disease Patients were Noticed in 2 Age Groups (Children Less than 12 Years and Adolescents Greater than 18 Years of Age).
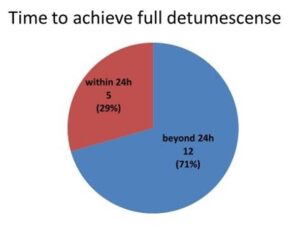
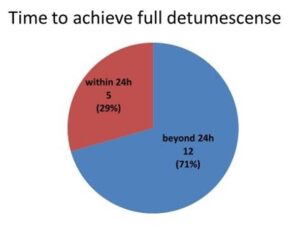
Following distal shunt procedures, all our patients have achieved full detumescense, however, post-operative intermittent massaging was required in those with recurrent tumescene after the surgeries in 71% of cases (Figure 4).
Figure 4: Pie chart showing the time within and beyond 24 hours to achieve detumescense following shunt procedure. Following the shunt procedures that were carried out, complete detumescense was achieved in 5 patients (29%) within 24 hours of surgery while in the remaining 12 (71%) it took more than 24 hours to get the penis flaccid. Intermittent penile massaging was employed after the shunts until the flaccid state was reached.
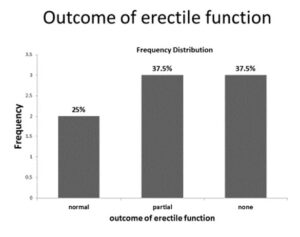
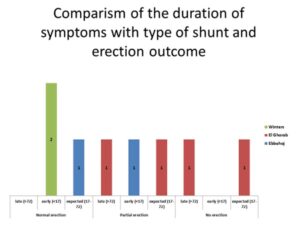
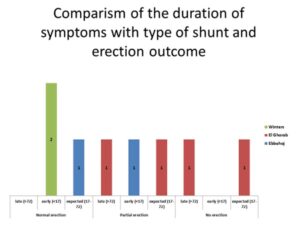
Priapism has been reported to carry a high risk (<35%) of erectile dysfunction.4 Twenty-five perecent of those who were sexually active before surgery reported normal erection adequate for penetrative intercourse despite delay in presentation (Figure 5). According to the suggestion of Aghaji and Badmus which state that despite the late presentation, vigorous surgical intervention should not be denied by the patients.2,3 Thirty seven point five percent had some erection inadequate for penetrative intercourse and another 37.5% had severe erectile dysfunction (Figure 5). Comparing the type of shunt procedure against the outcome on erectile function regardless of duration of symptoms, the winter shunt had the most likelihood of preservation of erectile function unlike the Ebbehoj and Al-Ghorab shunts (Figure 6). This series highlights the fact that late and delayed presentation of priapism is still rife in our environment and sickle cell disease remains a chief predisposing condition. Offering appropriate surgical intervention by the different way of shunt procedures, no matter how late, has the potential to preserve erectile function in some patients.><35%) of erectile dysfunction.4 Twenty-five perecent of those who were sexually active before surgery reported normal erection adequate for penetrative intercourse despite delay in presentation (Figure 5). According to the suggestion of Aghaji and Badmus which state that despite the late presentation, vigorous surgical intervention should not be denied by the patients. 2,3 Thirty seven point five percent had some erection inadequate for penetrative intercourse and another 37.5% had severe erectile dysfunction (Figure 5). Comparing the type of shunt procedure against the outcome on erectile function regardless of duration of symptoms, the winter shunt had the most likelihood of preservation of erectile function unlike the Ebbehoj and Al-Ghorab shunts (Figure 6). This series highlights the fact that late and delayed presentation of priapism is still rife in our environment and sickle cell disease remains a chief predisposing condition. Offering appropriate surgical intervention by the different way of shunt procedures, no matter how late, has the potential to preserve erectile function in some patients.
Figure 5: Bar Chart Depicting the Possible Outcomes of Erectile Function Following Shunt Procedures. Twenty-five percent and 37.5% of Patients had Normal and Partial Erections Respectively after Priapism and Shunt Procedures whereas another 37.5% Reported Loss of Erectile Function.
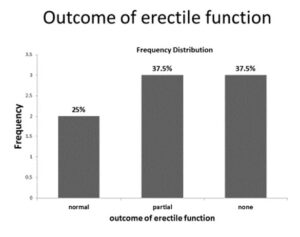
Figure 6: Comparison of the duration of Symptoms Prior to Surgery with Type of Shunt and Possible Outcome on Erection. Patients who Presented Earlier than 17 hours Following Onset of Priapism and had Winters Shunt were most likely to Maintain Normal Erections just as those who had Ebbehoj Shunt. All Patients Who had ElGhorab were those Who Presented after 17 Hours of Onset of Priapism and they all had no Erections. Those with Partial Erections had either El-Ghorab or Ebbehoj Procedures Regardless of Time of Presentation.
LIMITATIONS OF THE STUDY
Our series has a small number of cases and due to poor follow up attitude in our environment most of the patients were lost to follow-up thus limiting our duration of follow up to 3 months. Also a more objective method for assessing erectile function which is desirable could have been used but being a retrospective study we could only categorize the cases subjectively into full, partial and no erections.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.